We would like to acknowledge and thank our advising partner for their support in developing this toolkit:
- National Colorectal Cancer Roundtable, American Cancer Society. In particular, we’d like to thank Emily Bell, MPH, Director of the American Cancer Society National Colorectal Cancer Roundtable for her review and contributions.
About Colorectal Cancer Awareness Month
March is Colorectal Cancer Awareness Month and is an annual opportunity to raise awareness of colorectal cancer (CRC) and to promote research into its cause, prevention, diagnosis, screening, treatment, survivorship and cure. This toolkit can assist your organization in sharing important information with your networks about colorectal cancer.
Data and Statistics
141,902 new cases of colon and rectum cancer were reported in the US in 2021, the latest year in which comprehensive incidence data are available. For every 100,000 people, 36 new cases of colon and rectum cancer cases were reported. In 2022, the latest year mortality data are available, 52,967 people died of colorectal cancer. For every 100,000 people, 13 people died of colorectal cancer. Colorectal cancer is the fourth leading cause of cancer-related death in the US.[1] Because of health service disruptions throughout 2020 and 2021 due to the COVID-19 pandemic, cancer screening, diagnosis, and central cancer registry reporting may be delayed, and actual cancer occurrence may be underreported.
*Note about terminology: Here we report statistics the way in which they are reported in our source references, while emphasizing their limitations. Data are currently reported as binary sex data (male or female) and ignore gender and sex characteristic differences that make up the intersex spectrum, making it difficult to explain differences across gender and sexual orientations. While the latest North American Association of Central Cancer Registries (NAACCR) data dictionary includes multiple options beyond sex variables, the field may be underused or underreported. We advocate for systematic collection of sex assigned at birth, gender identity, sexual orientation, and intersex status to inform and advance evidence-based guidelines.
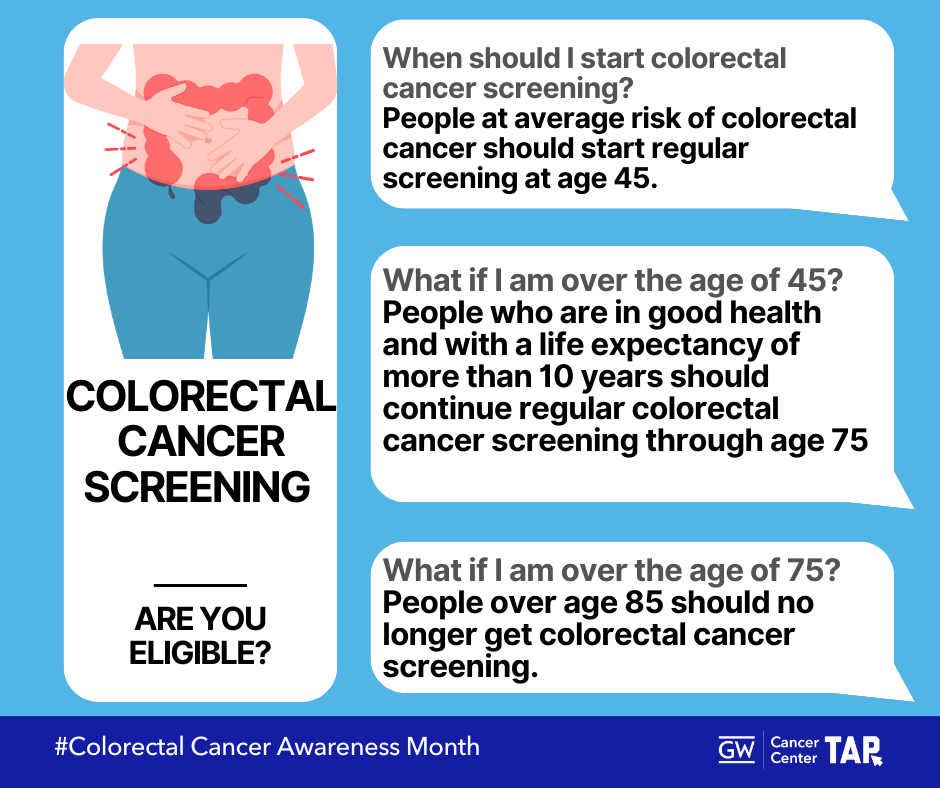
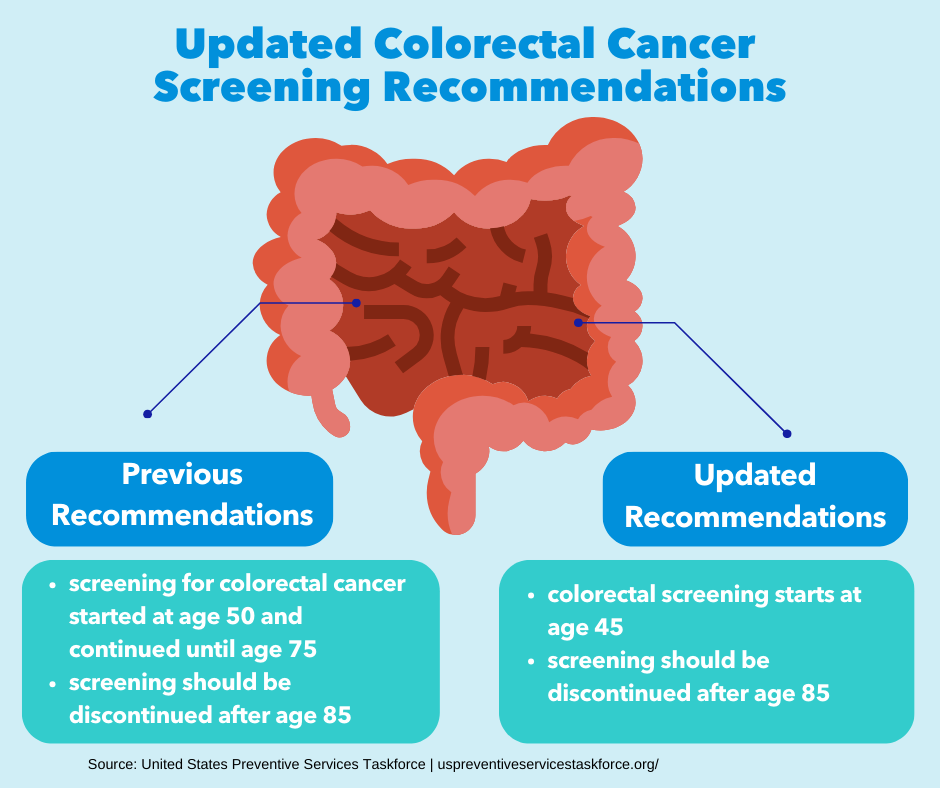
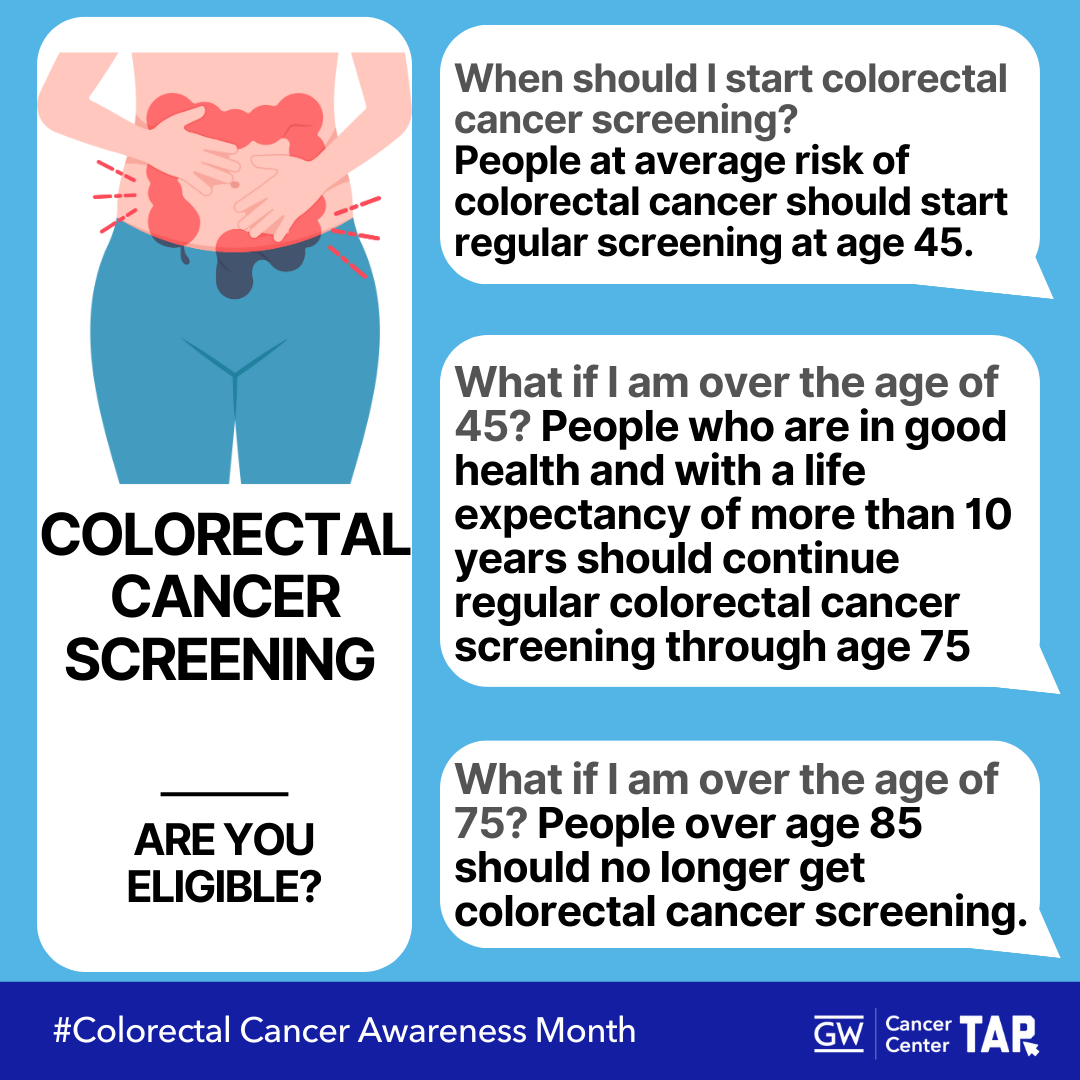
Screening Recommendations
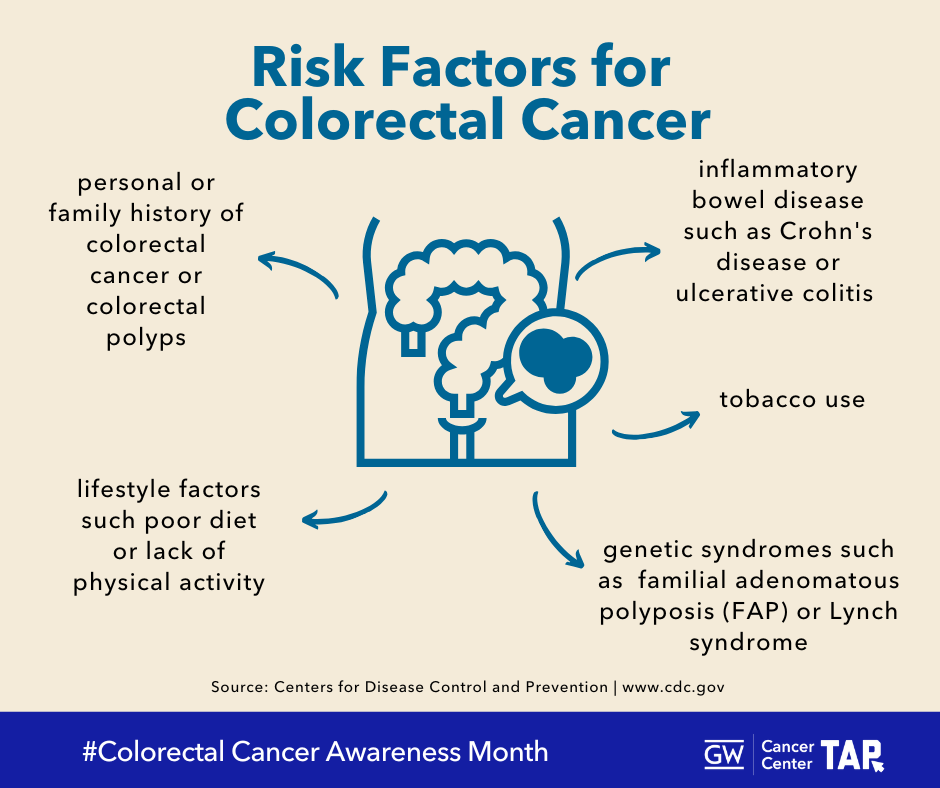
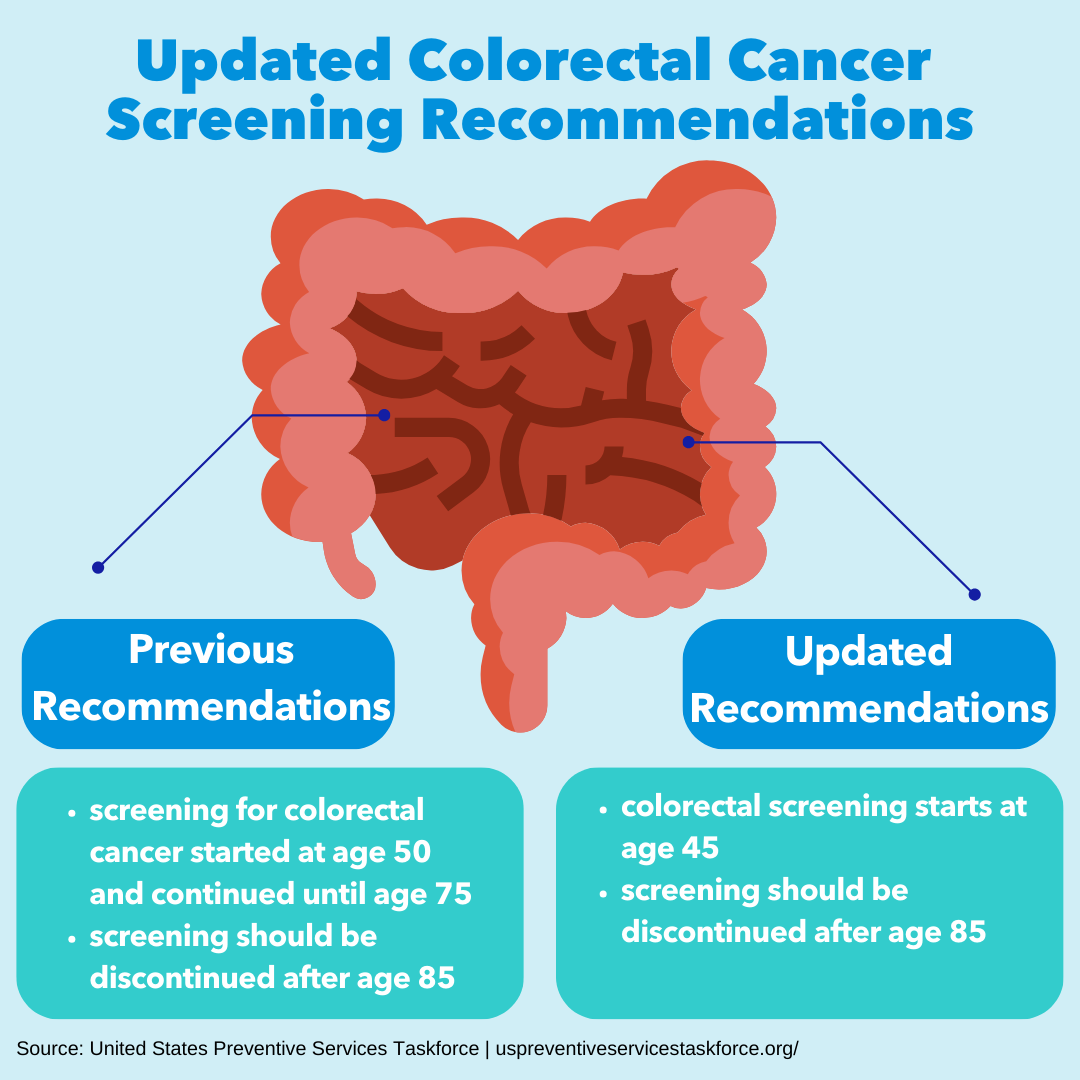
Screening is a proven tool to reduce the burden of colorectal cancer. Screening can detect cancer early, and can help detect and remove pre-cancerous polyps. As of 2021, the US Preventive Services Task Force (USPSTF) recommends screening for colorectal cancer in all adults aged 45 to 75 years. Some adults aged 76 to 85 may receive benefits from getting screened for colorectal cancer and should talk to their doctor about whether they should be screened.[2] People at increased or high risk of colorectal cancer may start colorectal cancer screening before age 45, be screened more often, and/or get specific screening tests.[3]
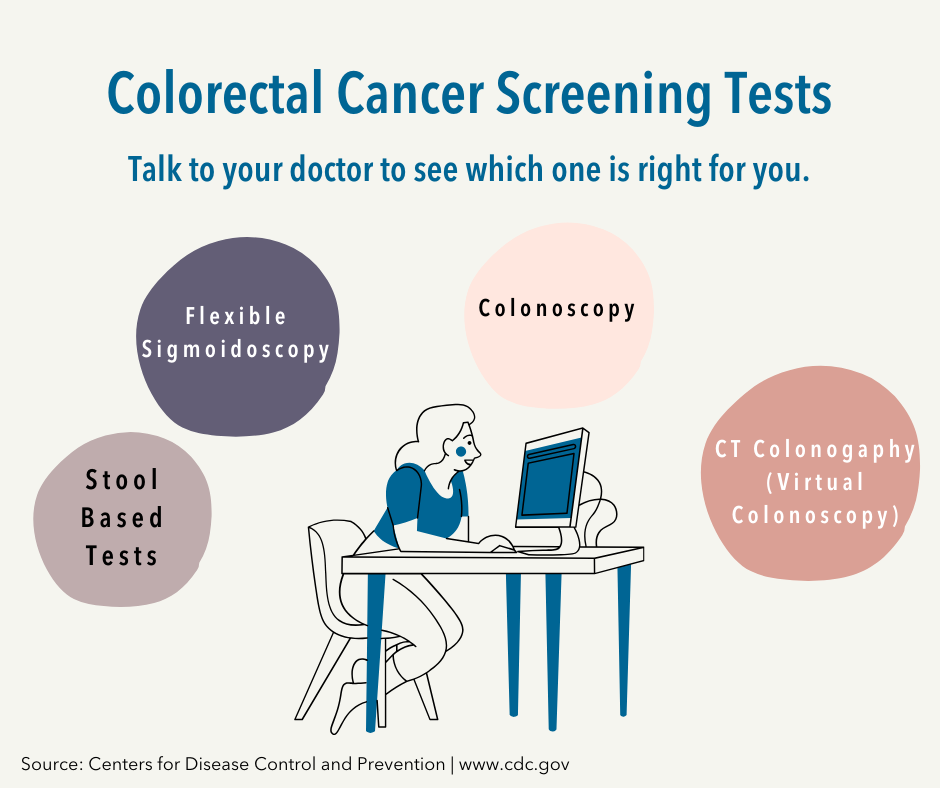
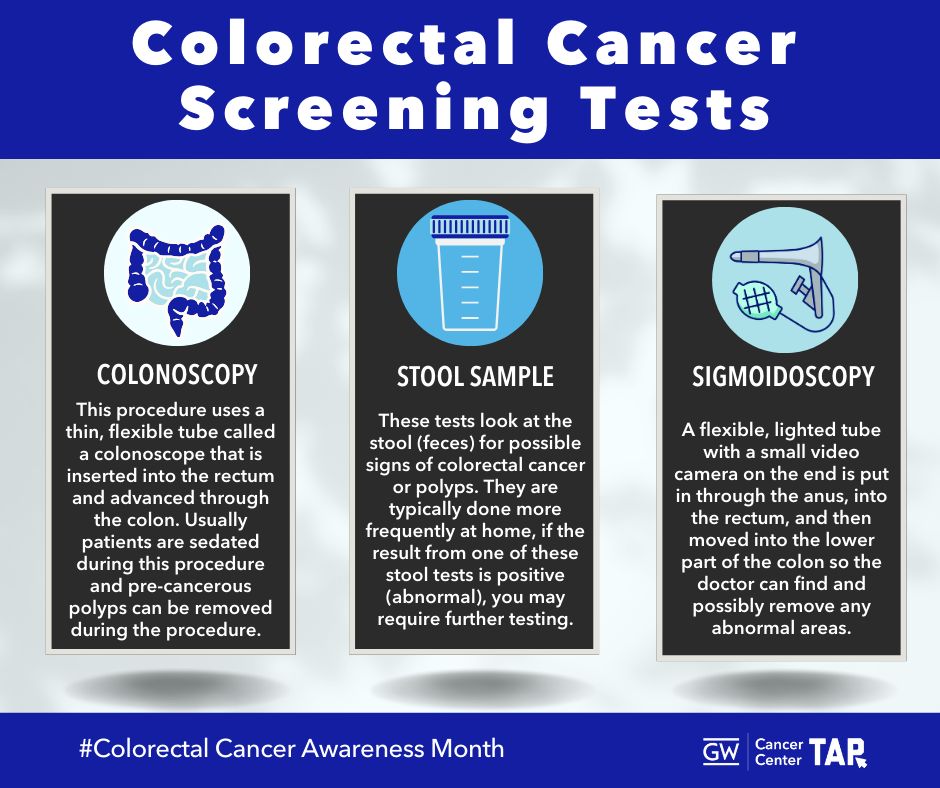
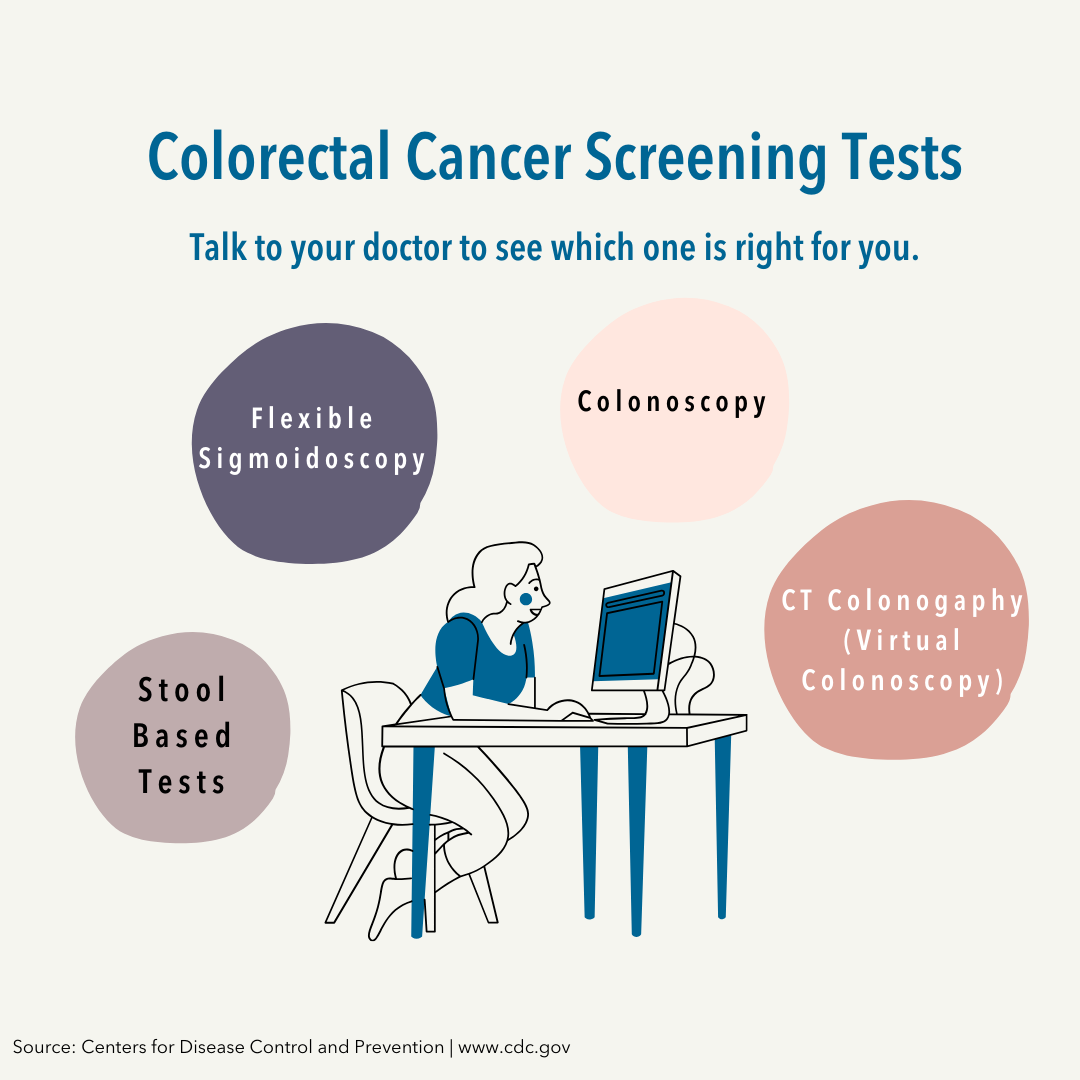
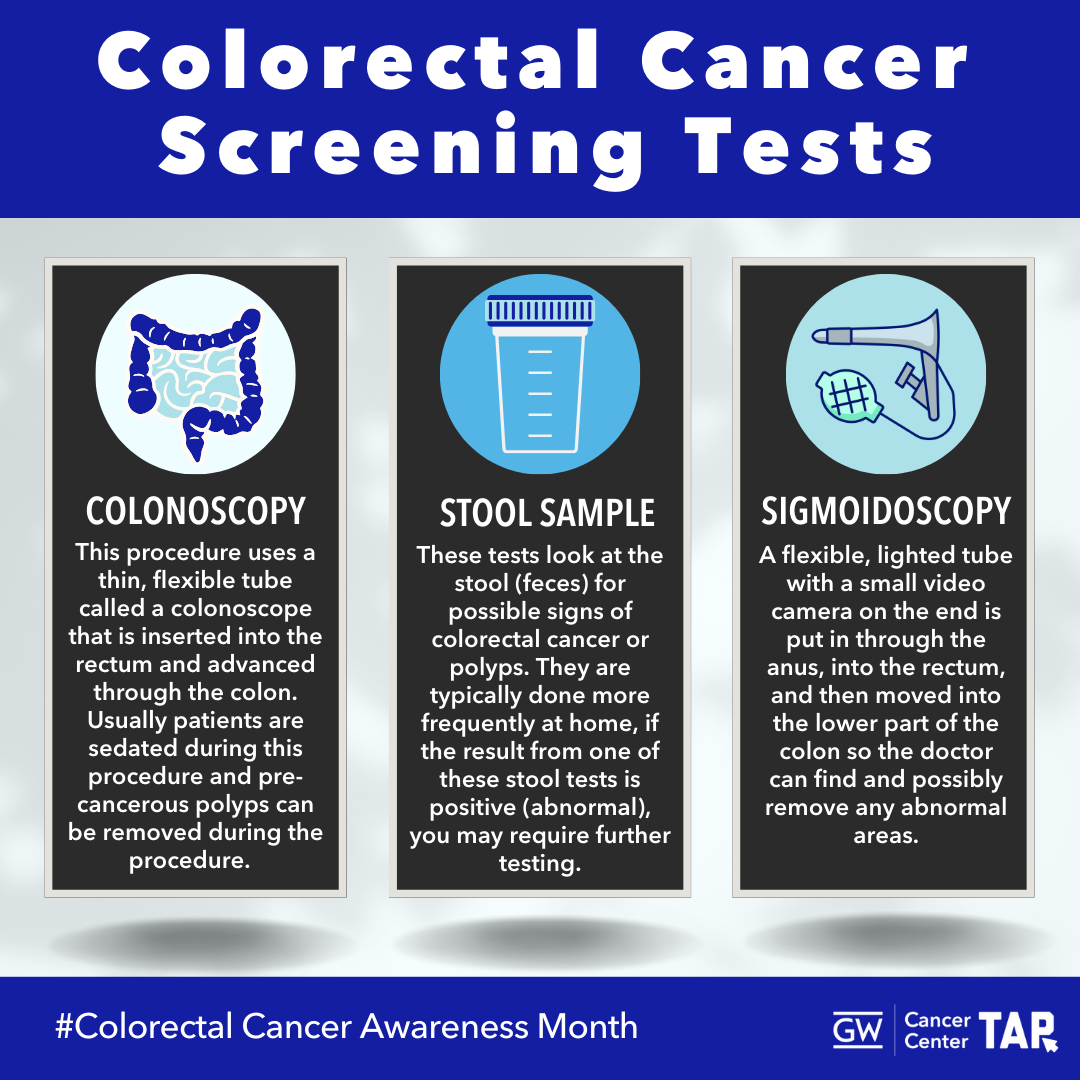
Several recommended screening tests are available. The US Preventive Services Task Force recommends stool-based tests like the high-sensitivity guaiac fecal occult blood test (gFOBT) or fecal immunochemical test (FIT) every year, and stool DNA tests (or sDNA-FIT) every one to three years, all of which can be more accessible tests as they are done from home.[4] Direct visualization tests are also recommended: colonoscopies are recommended every ten years, or the CT colonography and flexible sigmoidoscopy can be performed every five years. Doctors and patients may consider a wide variety of factors when deciding which test may be appropriate for each person.
Best Practices for Communicating About Colorectal Cancer
Use gender-neutral language, when possible. Current data is collected on reported sex (based on only two options: male or female) and does not necessarily correlate with the gender identity of those affected by cancer. Ensure language is inclusive; reflect the words used by your patients to refer to themselves as terminology evolves and varies across communities.
Address barriers to screening:
- Offer flexible screening options or at-home tests to accommodate for busy schedules.[5]
- Emphasize that screening can prevent cancer and save lives, especially for those that may fear results and outcomes.
- Highlight affordable or insurance-covered screening options.
- Educate on less invasive options like FIT or FOBT tests for those who may experience discomfort about procedures like colonoscopies.[6]
- Remind patients that CRC may not show symptoms early to dismiss concerns about perceived symptom requirements.
- Clarify that screening is still necessary even without a family history.
- Provide information about transportation services for screening.
- Connect patients with community health workers, patient navigators or social workers to help reduce barriers to screening and follow-up care.[7]
- Develop messaging that are plain-language and accessible: use alternative text in web graphics and ensure screen reader compatibility.
Promote Accessible Screening Options
- Use clear, simple messages to make screening information easy to understand and share across various platforms and communities.
- Highlight that screening helps prevent colorectal cancer by detecting precancerous polyps early, which can be removed before they develop into cancer.[8]
- Promote at-home tests, like FIT or FOBT, as a convenient option for individuals who may be hesitant about in-person visits. Include scheduling follow-up information for those that may experience barriers to colonoscopies after an abnormal screening result.[9]
- Offer information on various screening methods, including colonoscopy, sigmoidoscopy, and CT colonography, to ensure patients are aware of all available options.
- Reduce screening anxiety by emphasizing that at-home tests are a good first step and that additional testing, such as a colonoscopy, may be needed if the results are abnormal.[10]
- Ensure screening locations are physically accessible and offer accommodations, such as assistance for individuals who use mobility aids.
Promote Early and Regular Screening
- Encourage individuals under 45 to begin preparing for screening, to be aware of changes to their bowel movements, and emphasize the importance of early prevention, especially given the rise in early-age onset colorectal cancer.[11]
- Utilize ‘lead time messaging’ to prime adults under 45 to prepare for screening when they are eligible.[12] Resources like the ACS National Colorectal Cancer Roundtable’s Lead Time Messaging Guidebook can be a helpful tool for developing this language.
- Highlight the rising rates of colorectal cancer in younger adults and stress the importance of getting screened once they become eligible.
Use Personal Stories and Testimonials
- Share stories from individuals of various backgrounds and communities to make screening information more relatable and engaging to diverse audiences.[13]
- Leverage survivor narratives to demonstrate the life-saving impact of early detection and create a sense of urgency around screening.[14]
- Tailor personal stories to resonate with underserved populations, addressing their specific challenges and concerns regarding screening and prevention.[15]
Focus on Long-Term Care and Survivorship
- Promote personalized care plans that account for unique needs and preferences of patients, enabling tailored care approaches.
- Provide tailored resources for colorectal cancer survivors, including information on follow-up care, emotional support, and community resources.[16]
- Proactively address survivors’ psychological needs by offering referrals for mental health support and survivorship services to help them navigate life after treatment.[17]
- Encourage ongoing care by reminding survivors of the importance of regular check-ups to monitor for recurrence and ensure long-term health.
- Support sexual health by providing resources to address sexual and reproductive health concerns that may arise after treatment.
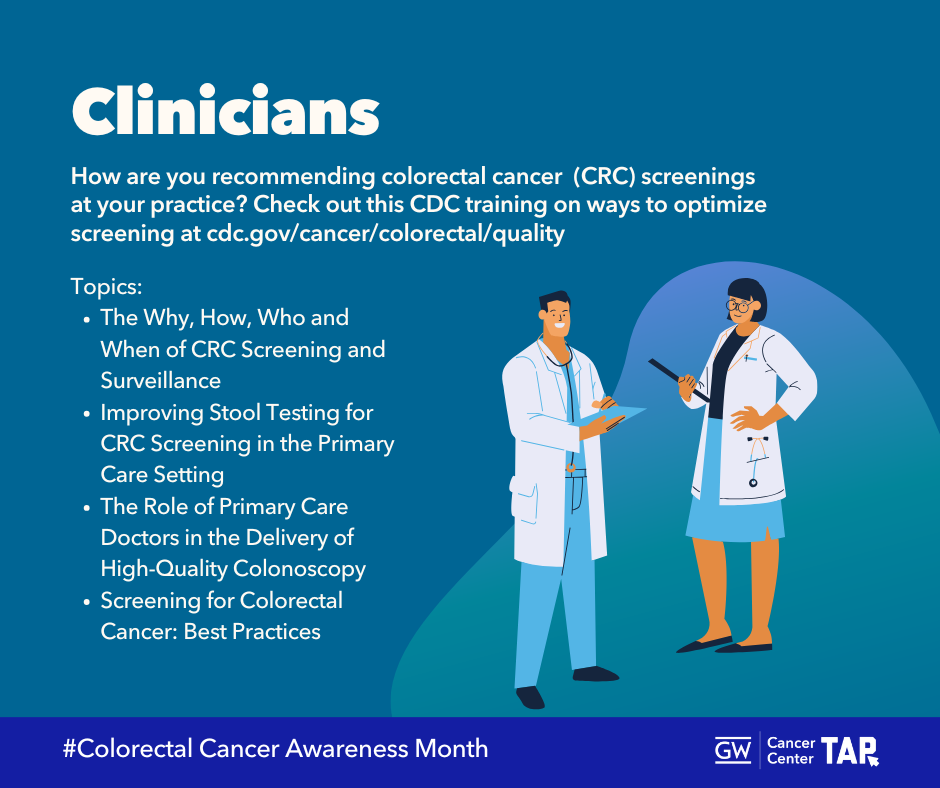
Healthcare Professional-Specific Recommendations
- Recommend and motivate patients to get screened, as lack of a clinician recommendation is a common barrier to colorectal cancer screening.[18]
- Explain screening options clearly to your patients and take the time to address any questions or concerns they may have.[19]
- Offer support for self-completed tests, such as FOBT, by sending reminders and assisting with the test process to ensure patients feel confident in completing the screening.[20]
- Promote shared decision-making by involving patients in their care, discussing their concerns, and providing evidence-based recommendations to guide their decisions.[21]
- Set up system reminders or text messaging systems to ensure patients receive follow-up notifications and complete their screenings on time.[22]
- Utilize patient navigators to increase screening rates, and assist patients who need follow-up care.
- Support colorectal cancer survivors through developing survivorship care plans.[23]
- Encourage patient navigation services for patients, which is proven to improve colorectal cancer screening rates.[24]
Communicating with Diverse Audiences
Certain groups experience disparities in CRC screening, incidence, mortality, and survival.[25] Cancer health disparities are complex and affected by various factors, such as social determinants of health, behavior, biology, genetics, and more. Consider the information most useful to each diverse group. When crafting communication campaigns for these groups, keep in mind that many individuals experience multiple forms of marginalization in and throughout health systems. This compounded experience of disadvantage, due to a variety of social identities, is referred to as intersectionality.
It is important to tailor communication and resources to these populations with messaging that also addresses conditions where these communities live, learn, work and play, as these factors can impact a wide range of health risks and outcomes.[26]
Colorectal Cancer Resources
| Resource | Description |
| Americans with Disability Act (ADA) National Network Resource Library | Resources from the ADA National Network provide detailed guidance on compliance with the ADA in healthcare settings, including accommodations for physical, sensory and cognitive disabilities. |
| Alliance for Disability in Medical Education | The Alliance for Disability in Medical Education provides resources to support professionals to enhance their practice to ensure cancer screening, treatment, and survivorship care is accessible, respectful and inclusive for all patients. |
| American Cancer Society – Education Materials for Your Patients | The American Cancer Society has a series of educational materials for clinicians to give to patients and caregivers, which are easy to read and on a variety of topics. |
| American Cancer Society Cancer Facts for Gay and Bisexual Men | The American Cancer Society has assembled a list of important cancer facts for Gay and Bisexual Men, including information on colorectal cancer. |
| American Indian Cancer Foundation: Colorectal Cancer Awareness | This foundation provides culturally-tailored infographics, toolkits and webinars to raise awareness of colorectal cancer among AI populations. |
| Clinician’s Reference: Stool-Based Tests for Colorectal Cancer Screening | This resource introduces clinicians to the value of stool-based testing for colorectal cancer and explains the different types available. |
| Colorectal Cancer Control Program (CRCCP) | The purpose of CDC’s Colorectal Cancer Control Program (CRCCP) is to increase colorectal cancer screening rates among people between 45 and 75 years of age by implementing evidence-based interventions described in the Guide to Community Preventive Services (the Community Guide) and other supporting strategies in partnership with health systems. They also provide follow-up services for a limited number of program-eligible people. |
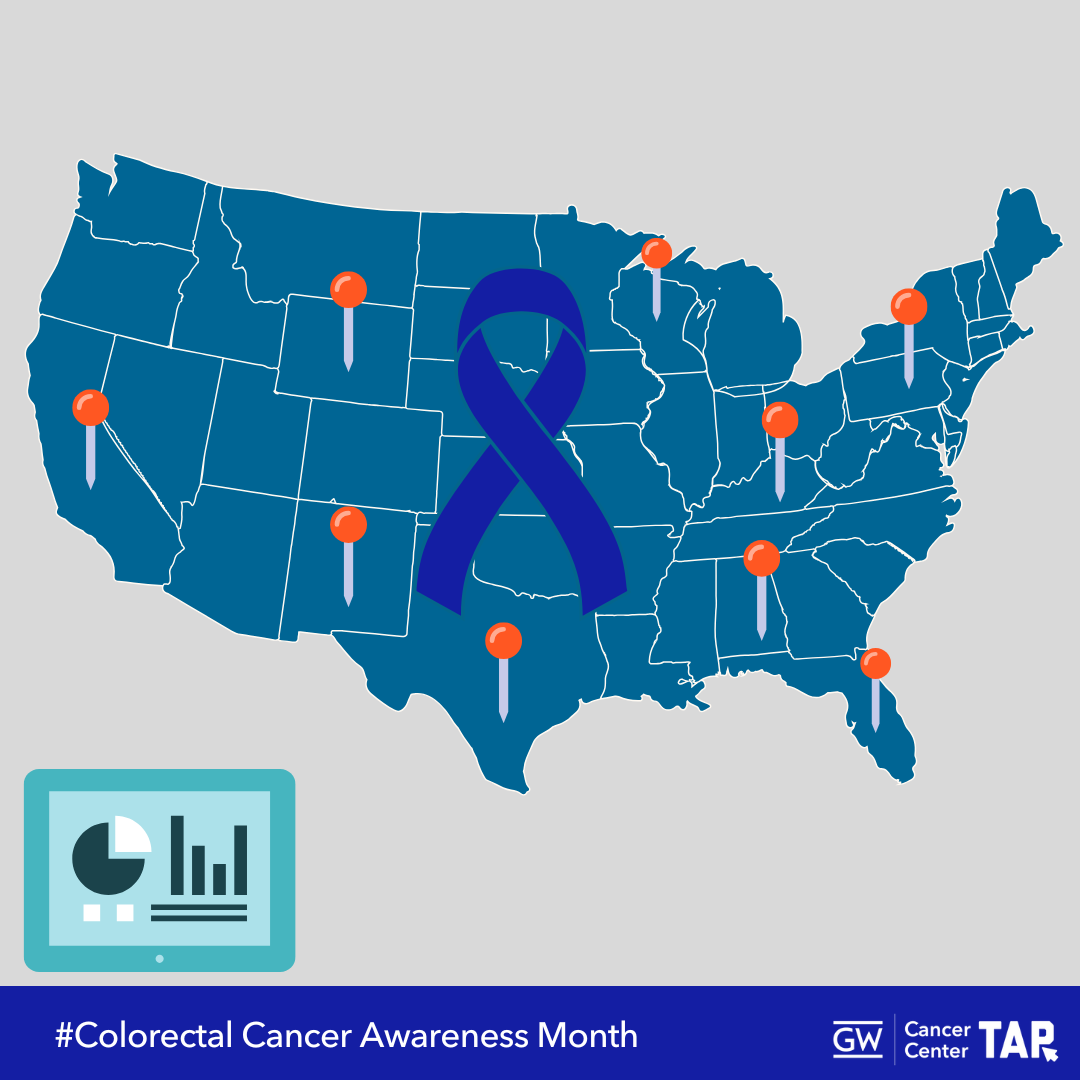
| Colorectal Cancer Data Dashboard | The American Cancer Society National Colorectal Cancer Roundtable’s Colorectal Cancer Data Dashboard (CRC Data Dashboard) offers an interactive view of data about colorectal cancer in the United States. |
| Colorectal Cancer: Early Detection, Diagnosis, and Staging | Find out how colorectal cancer is tested for, diagnosed, and staged with this webpage from the American Cancer Society. |
| Colon Cancer Videos | The videos in this collection explain colon cancer risk factors, screening tests, treatments, and personal stories from survivors. |
| Colorectal Cancer Screening in American Indian & Alaska Native Communities | This webinar, recorded on November 28, 2017, explored the opportunities and barriers related to delivering quality colorectal cancer screening and follow-up care in health care settings serving American Indian and Alaska Native (AI/AN) communities. |
| Colorectal Cancer Screening Best Practices: A Handbook for Hospitals and Health Systems | This source provides advice on the design and delivery of effective colorectal cancer screening interventions to strengthen overall efforts. |
| Colorectal Cancer Screening: What to Expect | Learn about three screening methods that can reduce risk of colorectal cancer: colonoscopy, sigmoidoscopy, and home stool test. |
| Comprehensive Cancer Control Plan Tip Sheet: Colorectal Cancer | This source from the American Cancer Society provides guidance on updating colorectal cancer screening in comprehensive cancer control plans, including information on engaging key partners, identifying data sources to measure efforts, and discussion questions surrounding colorectal cancer and screening. |
| Disability and Health Information | This resource from the CDC provides guidance on communicating with and providing services for individuals with disabilities, including accessibility standards for healthcare facilities. |
| The Dos and Don’ts of Colorectal Cancer Screening | A clinical resource to remind clinicians about dos and don’t of colorectal cancer screening. |
| GW Cancer Center: Together, Equitable, Accessible, Meaningful (TEAM) Training | This training aims to improve health equity by supporting organizational changes at the systems level. The training will help organizations implement quality improvements to advance equitable, accessible and patient-centered cancer care through improved patient-provider communication, cultural sensitivity, shared decision-making and attention to health literacy. |
| Increasing Colorectal Cancer Screening Among LGBTQ+ Communities Brief | This resource helps describe barriers to screening and outlines action steps to increase LGBTQ+ colorectal cancer screening. |
| My CT Colonography Center Locator Tool | The American College of Radiology (ACR) offers the My CT Colonography Center online locator, a patient-friendly online tool to find a computed tomography (CT) colonography screening center near you. |
| National Colorectal Cancer Roundtable (NCCRT) Learning Center | The new NCCRT Learning Center is a digital learning platform which features courses, tools and other resources on colorectal cancer screening delivery and research. |
| National LGBT Cancer Network Cancer Cards: English and Spanish Versions | These cards aim to raise awareness about colorectal, breast, lung, and cervical cancer among members of the LGBTQ+ community. There are also cards that address the need for taking care of an individual’s physical and mental health. Each bundle includes the front and the back of the cards in PDF format. |
| National LGBT Cancer Network OUT: The National Cancer Survey | The National LGBT Cancer Network released the findings from this survey in a report that provides information on experiences of LGBTQI cancer survivors and patients. Survey also includes a Special Sub-report on Gender Expansive Findings. |
| National LGBT Cancer Network Provider Databases | Directory of LGBTQ-welcoming cancer screening and treatment facilities across the U.S. |
| Screen for Life Campaign | Screen for Life is a CDC campaign to increase colorectal cancer screening among men and women ages 45 or older. The campaign provides free print materials (fact sheets, brochures, postcards, etc.), TV and radio PSAs, social media posts and images, and other materials in English and Spanish to inform men and women about the importance of colorectal cancer screening. |
| Asian Americans and Colorectal Cancer Companion Guide | This companion guide reviews what we know from market research about unscreened Asian Americans and introduces and explains new tested messages. |
| CDC Colorectal Cancer Communication Resources | CDC offers scientifically accurate information about colorectal cancer in a variety of formats. |
| Mailed FIT Outreach for Colorectal Cancer Screening | This research tests ways to deliver mailed FIT outreach and support follow-up colonoscopy for populations that face barriers to screening. It includes graphics and videos on colorectal cancer screenings. |
| State-By-State Colorectal Cancer Screening Landscape | This resource (last updated in 2020) is a snapshot of the colorectal cancer screening landscape in each state while also putting into context how the different states compare with each other in a range of areas. Includes information on coverage, screening rates and legislation. |
| State Cancer Profiles | The State Cancer Profiles website provides interactive graphics and maps to characterize the cancer burden across various geographic areas and demographic groups. It focuses on cancer sites for which there are evidence-based control interventions. |
| Tailoring Colorectal Cancer Screening Messaging: A Practical Coalition Guide | This resource, designed for coalition members and leaders, helps create tailored health messaging for colorectal cancer screening. |
| Hispanics/Latinos and Colorectal Cancer Companion Guide | This companion guide reviews what we know from market research about unscreened Hispanics/ Latinos and introduces and explains new tested messages. |
| What Can LGBT Communities Do to Advance Colorectal Cancer Screening? | Learn four things you can do to support reaching colorectal cancer screening rates of 80% and higher in LGBT communities. |
| Your Colon is 45 | This initiative directs users to a quiz for a personalized screening letter and screening locater for colorectal cancer. It also has several social media graphics and posts to promote on-time screening. |
| 2022 Messaging Guidebook for Black & African American People: Messages to Motivate for Colorectal Cancer Screening | This guidebook provides tools and information for screening messaging to close disparity gaps in colorectal cancer screening. |
| 2023 Lead Time Messaging Guidebook | This guidebook shares recommendations about tailored messages to encourage on-time and regular colorectal cancer screening. |
| Cheeky Charity | Cheeky Charity promotes information on colorectal and anal cancer prevention and early detection, especially for the LGBTQ+ and younger communities. A queer-led organization with a ‘cheeky’ approach that gets people talking, learning, and taking action. |
| Colorectal Cancer Alliance | The Colorectal Cancer Alliance is the nation’s leading nonprofit dedicated to colorectal cancer. Together with a nation of passionate allies, we advocate for prevention, magnify support, and accelerate research to end this disease |
| National Cancer Institute | National Cancer Institute Colorectal Cancer Patient Information and Health Professional Version |
Colorectal Cancer Awareness Month Messages and Graphics
Twitter/X
Download All Messages and Graphics
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheet below can be adapted to fit multiple scheduling platforms or services. It is currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
If you would like to download all images in this social media toolkit, click on each network below for a zip file with each network’s graphics. Please note that these image sizes are slightly smaller than the links above due to file size limitations. If you would like to download full resolution versions, simply click on the “Download Graphic” link below each image in the message tables above.
Template Graphics
Need to adjust our designs? Use our Canva Templates for GW TAP’s Colorectal Cancer Awareness Month Graphics
References
1. U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention (2021). United States Cancer Statistics Working Group, U.S. Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999-2018). Retrieved from https://gis.cdc.gov/Cancer/USCS/DataViz.html
2. U.S. Preventive Services Task Force. (2021). Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA, 325(19),1965-1977. http://dx.doi.org/10.1001/jama.2021.6238
3. American Cancer Society (2024). American Cancer Society Guideline for Colorectal Cancer Screening. https://www.cancer.org/cancer/types/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html
4. U.S. Preventive Services Task Force, 2021.
5. U.S. Preventive Services Task Force, 2021; National Colorectal Cancer Roundtable (2019). 2019 Colorectal Cancer Screening Message Guidebook. https://nccrt.org/resource/2019messagingguidebook/ ; Kerrison, R. S., Travis, E., Dobson, C., Whitaker, K. L., Rees, C. J., Duffy, S. W., & von Wagner, C. (2022). Barriers and facilitators to colonoscopy following fecal immunochemical test screening for colorectal cancer: A key informant interview study. Patient education and counseling, 105(6), 1652–1662. https://doi.org/10.1016/j.pec.2021.09.022
6. Scaglioni, G., Guidetti, M., & Cavazza, N. (2021). The role of disgust as an emotional barrier to colorectal cancer screening participation: a systematic review and meta-analysis. Psychology & Health, 38(3), 389–408. https://doi.org/10.1080/08870446.2021.1967351
7. Nelson, H. D., Cantor, A., Wagner, J., Jungbauer, R., Fu, R., Kondo, K., Stillman, L., & Quiñones, A. (2020). Effectiveness of Patient Navigation to Increase Cancer Screening in Populations Adversely Affected by Health Disparities: a Meta-analysis. Journal of general internal medicine, 35(10), 3026–3035. https://doi.org/10.1007/s11606-020-06020-9
8. Small, C., Raymond, V., Jacobstein, M., Lang, K. (2020). Understanding patient-reported barriers to colorectal cancer screening: A literature review. Cancer Epidemiol Biomarkers Prev 2020: 29(6 Suppl 2). http://dx.doi.org/10.1158/1538-7755.DISP19-B051; National Colorectal Cancer Roundtable, 2019.
9. Kerrison, R. S., Travis, E., Dobson, C., Whitaker, K. L., Rees, C. J., Duffy, S. W., & von Wagner, C. (2022). Barriers and facilitators to colonoscopy following fecal immunochemical test screening for colorectal cancer: A key informant interview study. Patient education and counseling, 105(6), 1652–1662. https://doi.org/10.1016/j.pec.2021.09.022
10. Centers for Disease Control and Prevention (2021). Colorectal Cancer Screening Tests. Retrieved from https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
11. American Cancer Society. (2024). Cancer Facts & Figures 2024. Retreived from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2024/2024-cancer-facts-and-figures-acs.pdf
12. American Cancer Society National Colorectal Cancer Roundtable. (2023). Lead Time Messaging Guidebook. Retrieved from https://nccrt.org/wp-content/uploads/2023/12/2023-Lead-Time-Messaging-Guidebook-v15.pdf
13. National Colorectal Cancer Roundtable, 2019.
14. McQueen, A., Caburnay, C., Kreuter, M., & Sefko, J. (2019). Improving Adherence to Colorectal Cancer Screening: A Randomized Intervention to Compare Screener vs. Survivor Narratives. Journal of Health Communication, 24(2), 141-155. http://dx.doi.org/10.1080/10810730.2019.1587109
15. Woudstra, A. J., & Suurmond, J. (2019). How narratives influence colorectal cancer screening decision making and uptake: A realist review. Health expectations: an international journal of public participation in health care and health policy, 22(3), 327–337. https://doi.org/10.1111/hex.12892
16. American Cancer Society. (2024). Living as a Colorectal Cancer Survivor. Retrieved from https://www.cancer.org/cancer/types/colon-rectal-cancer/after-treatment/living.html
17. Luo, X., Li, J., Chen, M., Gong, J., Xu, Y., & Li, Q. (2021). A literature review of post-treatment survivorship interventions for colorectal cancer survivors and/or their caregivers. Psycho-oncology, 30(6), 807–817. https://doi.org/10.1002/pon.5657
18. Small et al., 2020.
19. Vallone, F., Lemmo, D., Martino, M. L., Donizzetti, A. R., Freda, M. F., Palumbo, F., Lorenzo, E., D’Argenzio, A., & Caso, D. (2022). Factors promoting breast, cervical and colorectal cancer screenings participation: A systematic review. Psycho-oncology, 31(9), 1435–1447. https://doi.org/10.1002/pon.5997
20. Kotzur M, McCowan C, Macdonald S.. (2020). Why colorectal screening fails to achieve the uptake rates of breast and cervical cancer screening: a comparative qualitative study. BMJ Qual Saf 2020 (29), 482–490. https://doi.org/10.1136/bmjqs-2019-009998
21. Kindratt, T.B., Atem, F., Dallo, F. J., Allicock, M., & Balasubramanian, B. A. (2020). The Influence of Patient–Provider Communication on Cancer Screening. Journal of Patient Experience, 7(6), 1648–1657. https://doi.org/10.1177/2374373520924993
22. Fendrick, A. M., Fisher, D. A., Saoud, L., Ozbay, A. B., Karlitz, J. J., & Limburg, P. J. (2021). Impact of Patient Adherence to Stool-Based Colorectal Cancer Screening and Colonoscopy Following a Positive Test on Clinical Outcomes. Cancer prevention research, 14(9), 845–850. https://doi.org/10.1158/1940-6207.CAPR-21-0075 ; Bai, Y., Wong, C. L., He, X., Wang, C., & So, W. K. W. (2020). Effectiveness of tailored communication intervention in increasing colonoscopy screening rates amongst first-degree relatives of individuals with colorectal cancer: A systematic review and meta-analysis. International journal of nursing studies, 101, 103397. https://doi.org/10.1016/j.ijnurstu.2019.103397
23. American Cancer Society, 2024.
24. Nelson et al. 2020.
25. National Cancer Institute. (2020). Cancer disparities. Retrieved from https://www.cancer.gov/about-cancer/understanding/disparities
26. Centers for Disease Control and Prevention (2021). About Social Determinants of Health (SDOH). Retrieved from https://www.cdc.gov/socialdeterminants/about.html
27. American Cancer Society (2020). Colorectal Cancer Facts and Figures 2020-2022. Atlanta: American Cancer Society, 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2020-2022.pdf
28. Sabatino S.A., Thompson T.D., White M.C., Shapiro, J.A., De Moor, J., Doria-Rose, P., Clarke, T., Richardson, L.C. (2021). Cancer Screening Test Receipt — United States, 2018. MMWR Morb Mortal Wkly Rep 2021; 70:29–35. http://dx.doi.org/10.15585/mmwr.mm7002a1
29. Syvyk, S., Roberts, S. E., Finn, C. B., Wirtalla, C., & Kelz, R. (2022). Colorectal cancer disparities across the continuum of cancer care: A systematic review and meta-analysis. American journal of surgery, 224(1 Pt B), 323–331. https://doi.org/10.1016/j.amjsurg.2022.02.049
30. ACS, 2020.
31. ACS, 2020.
32. American Cancer Society (2021). Cancer Facts & Figures for Hispanic/Latino People 2021-2023. Atlanta: American Cancer Society, 2021. https://www.cancer.org/research/cancer-facts-statistics/hispanics-latinos-facts-figures.html
33. Miller, K.D., Ortiz, A.P., Pinheiro, P.S., Bandi, P., Minihan, A., Fuchs, H.E., Martinez Tyson, D., Tortolero-Luna, G., Fedewa, S.A., Jemal, A.M., Siegel, R.L. (2021). Cancer statistics for the US Hispanic/Latino population, 2021. CA Cancer J Clin. 2021: 71: 466- 487. https://doi.org/10.3322/caac.21695
34. ACS, 2021.
35. Miller et al. 2021.
36. American Cancer Society. (2024). Cancer Facts & Figures for Hispanic/Latino People 2024-2026. Atlanta: American Cancer Society. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/2024/2024-2026-cancer-facts-and-figures-for-hispanics-and-latinos.pdf
37. National Colorectal Cancer Roundtable (2019). 2019 Colorectal Cancer Screening Message Guidebook. https://nccrt.org/resource/2019messagingguidebook/
38. Shah, I., Gawron, A. J., Byrne, K. R., & Inadomi, J. M. (2024). Disparities in Colorectal Cancer Screening Among Asian American Populations and Strategies to Address These Disparities. Gastroenterology, 166(4), 549–552. https://doi.org/10.1053/j.gastro.2024.02.009
39. Chun, I, Brenda Y. Hernandez, Hyeong Jun Ahn, and Christina Wai. (2024). Disaggregating U.S. Asian and Pacific Islanders: Colorectal cancer. Surgical Oncology Insight, 1(3). https://doi.org/10.1016/j.soi.2024.100066
40. Sabatino et al. 2021.
41. Oh, K. M., An, K., Lee, M., Shin, C., & Steves, S. L. (2023). Colorectal cancer screening disparities in Asian Americans: the influences of patient-provider communication and social media use. Cancer causes & control : CCC, 34(9), 813–827. https://doi.org/10.1007/s10552-023-01720-z
42. Medina, H. N., Callahan, K. E., Morris, C. R., Thompson, C. A., Siweya, A., & Pinheiro, P. S. (2021). Cancer Mortality Disparities among Asian American and Native Hawaiian/Pacific Islander Populations in California. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 30(7), 1387–1396. https://doi.org/10.1158/1055-9965.EPI-20-1528
43. Chun et al. 2024.
44. Medina et al. 2021.
45. Chun et al. 2024.
46. U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention (2021). United States Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999-2018): American Indian and Alaska Native restricted to PRCDA only. Retrieved from https://gis.cdc.gov/Cancer/USCS/#/AIAN/
47. Sabatino et al. 2021.
48. Haverkamp, D., English, K., Jacobs-Wingo, J., Tjemsland, A., & Espey, D. (2020). Effectiveness of Interventions to Increase Colorectal Cancer Screening Among American Indians and Alaska Natives. Preventing Chronic Disease, 17, E62–E62. https://doi.org/10.5888/pcd17.200049
49. Sabatino et al., 2021.
50. NCCRT, 2019.
51. NCCRT, 2019.
52. Kratzer, T. B., Star, J., Minihan, A. K., Bandi, P., Scout, N. F. N., Gary, M., Riddle-Jones, L., Giaquinto, A. N., Islami, F., Jemal, A., & Siegel, R. L. (2024). Cancer in people who identify as lesbian, gay, bisexual, transgender, queer, or gender-nonconforming. Cancer, 130(17), 2948–2967. https://doi.org/10.1002/cncr.35355
53. National LGBT Cancer Network (2021). OUT: The National Cancer Survey, Summary of Findings. https://cancer-network.org/out-the-national-cancer-survey/
54. National LGBT Cancer Network, 2021.
55. Sepassi, A., Li, M., Zell, J. A., Chan, A., Saunders, I. M., & Mukamel, D. B. (2024). Rural-Urban Disparities in Colorectal Cancer Screening, Diagnosis, Treatment, and Survivorship Care: A Systematic Review and Meta-Analysis. The oncologist, 29(4), e431–e446. https://doi.org/10.1093/oncolo/oyad347
56. Lee, K. M. N., Hunleth, J., Rolf, L., Maki, J., Lewis-Thames, M., Oestmann, K., & James, A. S. (2023). Distance and Transportation Barriers to Colorectal Cancer Screening in a Rural Community. Journal of primary care & community health, 14, 21501319221147126. https://doi.org/10.1177/21501319221147126
57. Lee et al. 2023.
58. Santiago-Rodríguez, E. J., Rivadeneira, N. A., Torres, J. M., Sarkar, U., & Hiatt, R. A. (2022). Socioeconomic status and colorectal cancer screening behaviors in a vulnerable multiethnic population. Ethnicity & health, 27(4), 980–996. https://doi.org/10.1080/13557858.2020.1838454
59. Carethers, J. M., & Doubeni, C. A. (2020). Causes of Socioeconomic Disparities in Colorectal Cancer and Intervention Framework and Strategies. Gastroenterology, 158(2), 354–367. https://doi.org/10.1053/j.gastro.2019.10.029
60. Ricciardi, G. E., Cuciniello, R., De Ponti, E., Lunetti, C., Pennisi, F., Signorelli, C., & Renzi, C. (2024). Disability and Participation in Colorectal Cancer Screening: A Systematic Review and Meta-Analysis. Current oncology (Toronto, Ont.), 31(11), 7023–7039. https://doi.org/10.3390/curroncol31110517
61. Ricciardi et al. 2024.
52. Satgé, D., Habib-Hadef, S., Otandault, A., Samalin, E., & Trétarre, B. (2023). Advocacy for colorectal cancer screening and awareness in people with intellectual disability. Journal of gastrointestinal oncology, 14(3), 1650–1652. https://doi.org/10.21037/jgo-22-998
63. Hughes, R. B., Robinson-Whelen, S., & Knudson, C. (2022). Cancer Disparities Experienced by People with Disabilities. International journal of environmental research and public health, 19(15), 9187. https://doi.org/10.3390/ijerph19159187
64. Iezzoni L. I. (2022). Cancer detection, diagnosis, and treatment for adults with disabilities. The Lancet. Oncology, 23(4), e164–e173. https://doi.org/10.1016/S1470-2045(22)00018-3 [1] Kim, K. B., Shin, D. W., Yeob, K. E., Kim, S. Y., Han, J. H., Park, S. M., Park, J. H., & Park, J. H. (2024). Disparities in the diagnosis and treatment of colorectal cancer among patients with disabilities. World journal of gastrointestinal oncology, 16(7), 2925–2940. https://doi.org/10.4251/wjgo.v16.i7.2925
65. Kim, K. B., Shin, D. W., Yeob, K. E., Kim, S. Y., Han, J. H., Park, S. M., Park, J. H., & Park, J. H. (2024). Disparities in the diagnosis and treatment of colorectal cancer among patients with disabilities. World journal of gastrointestinal oncology, 16(7), 2925–2940. https://doi.org/10.4251/wjgo.v16.i7.2925