Gynecological Cancer
Gynecological cancer refers to any cancer that originates in a female reproductive organ, such as ovarian, cervical, uterine/endometrial, vaginal, and vulvar cancers.1 These cancers have varying symptoms, and as screenings are not available for these cancers except for cervical cancer, it is important for patients and providers to understand and recognize the symptoms for each. This health awareness campaign can help your organization implement evidence-based practices when communicating about gynecological cancer.
Data and Statistics
In 2019, the latest year for which incidence data are available in the U.S., for every 100,000 females, 28 new uterine cancer cases, eight new cervical cancer cases, and ten new ovarian cases were reported.2
Uterine—specifically endometrial—is the most common gynecologic cancer while vaginal is the least common.3 Uterine cancer includes the more common endometrial cancer and the rarer uterine sarcoma.3 Of the gynecological cancers, ovarian cancer is responsible for the most deaths among individuals assigned female at birth in the United States.4
Best Practices for Communicating About Gynecological Cancer
Communicating with Diverse Audiences
Communication-related issues may also play a role in cancer disparities.19 Consider the information most useful to each diverse group (see below for specific messaging and read more on health disparities here). Tailor communication to these populations of focus with messages that also address conditions where these communities live, learn, work and play, as these social determinants of health can impact a wide range of health risks and outcomes. To ensure messages resonate with the coalition’s intended audience, we also recommend referring to the National Networks’ existing resources and adapting messages to reflect individuals with lived experiences.
Gynecological Cancer Messages and Graphics
Download All Messages and Graphics How to Post on Social Media
| Topics | Suggested Images |
|---|---|
| Topic: Helping patients understand risk factors for ovarian cancer Providers, are your patients at higher risk of ovarian cancer? Certain comorbidities and family histories are associated with higher cancer incidences. Remember to communicate these risk factors with high-risk patients. #cctgynecology #gynocancer #ovariancancer #cdc #dcpc |  |
| Topic: Promoting healthy behaviors for survivors In addition to maintaining checkups and screenings, survivors can implement several lifestyle changes to keep themselves healthy and happy. This survivorship guide from the Foundation for Women’s Cancer can provide patients with a groundwork for making healthier choices. http://bitly.ws/KEE2 #cctgynecology #gynocancer #cancersurvivor #cdc #dcpc |  |
| Topic: Giving survivors the tools to monitor their own health #DidYouKnow that the Society of Gynecologic Oncology provides a Survivorship Toolkit so that patients can champion their own health? These include potential side effects of treatment for each type of gynecologic cancer, recommended follow-up intervals, and a self-care plan. https://bit.ly/3zsXQjJ #cctgynecology #gynocancer #cancersurvivor #cdc #dcpc |  |
| Topic: Give providers resources to find appropriate gynecologic cancer clinical trials Limited data on Black and other persons of color with gynecologic cancer is a barrier to achieving racial health equity. You can help to create change by engaging persons of color, particularly Black women, in gynecologic cancer clinical trials. Use EmergingMed’s online tool to find relevant trials: https://bit.ly/3Kz6WBU #cctgynecology #gynocancer #cancertrials #cdc #dcpc |  |
| Topic: Sharing resources for non-English speaking patients Do you have gynecologic patients who speak Spanish or Chinese? The Foundation for Women’s Cancer provides resource booklets in English, Spanish, and Chinese that cover cancer screenings, survivorship care, clinical trial participation, and more. https://bit.ly/3Gh66qB #cctgynecology #gynocancer #cdc #dcpc |  |
| Topic: Tips for caring for LGBTQI+ patients Caring for LGBTQI+ patients requires knowing how to communicate respectfully and making them feel at ease. When engaging patients with gynecological cancer, remember these strategies from the National LGBT Cancer Network for creating a welcoming environment. #cctgynecology #gynocancer #lgbtcancer #cdc #dcpc |  |
| Topic: Tips for caring for transgender patients How you engage transgender patients with gynecological cancer could play a critical role in whether they continue to seek necessary health screenings and treatments. Consider these recommendations for transgender inclusivity from the National LGBT Cancer Network. #cctgynecology #gynocancer #lgbtcancer #transhealth #cdc #dcpc |  |
| Topic: Considering the effects of hormone therapies when caring for transgender patients #DidYouKnow that transgender patients who take testosterone are at elevated risk for HPV? Discuss and encourage high-risk HPV testing with transgender patients who were assigned female at birth. For those who have not undergone gender-affirming surgery, encourage additional screening for cervical cancers. #cctgynecology #gynocancer #lgbtcancer #transhealth #cdc #dcpc |  |
| Topic: Encourage cervical cancer screenings for American Indian and Alaska Native patients Despite advances in prevention strategies, American Indian and Alaska Native patients continue to experience higher incidences of cervical cancer and higher cervical cancer mortality rates. Encourage AI/AN patients to screen for cervical cancer even before symptoms have appeared. If precancerous cells are detected, preliminary treatments can stop cancer from developing. #cctgynecology #gynocancer #cervicalcancer #aian #cdc #dcpc |  |
| Topic: Uterine cancer awareness for Black patients Despite experiencing similar rates of uterine cancer, mortality rates for Black persons are higher than those of White persons. Per 100,000 people, 9 Black patients will die of uterine cancer, as compared to 5 White patients. Sharing this data and these common uterine cancer symptoms can help Black patients seek diagnosis at an earlier stage. #cctgynecology #gynocancer #uterinecancer #blackhealth #cdc #dcpc |  |
| Topic: Cervical cancer awareness for Hispanic patients Hispanic patients experience a higher incidence rate of cervical cancer compared to other racial/ethnic groups. Fortunately, screenings can help with early detection and can improve the chances of survival. Encourage Hispanic patients to know the symptoms of cervical cancer and to keep up with routine screenings. #cctgynecology #gynocancer #latinxcancer #cdc #dcpc |  |
| Topic: Encourage age-based cervical cancer screenings A patient’s age determines how frequently they should be screened for cervical cancer. These cancer.gov guidelines can help you set a framework for maintaining appropriate screenings and check-ups for patients. Remember that patients who are HIV positive or have a cancer history may require more frequent testing. #cctgynecology #gynocancer #cervicalcancer #cancerscreening #cdc #dcpc |  |
| Topic: Encourage HPV vaccinations for adolescents and young adults #DidYouKnow that HPV vaccinations can be recommended and started at age 9? Receiving all doses of the vaccine can help to prevent cancers that are commonly linked to HPV, such as cervical, vaginal, and vulvar cancers. This CDC guide can help you navigate conversations about HPV vaccines with parents of adolescents and young adults. https://bit.ly/40ACiwD #cctgynecology #gynocancer #hpv #cdc #dcpc |  |
| Topic: Share family-planning and fertility resources No matter a patient’s age or diagnosis, it’s important to discuss fertility preservation and family planning—especially when treatment of gynecological cancers will affect reproductive organs. SaveMyFertility.org offers pocket guides for both providers and patients to assist with navigating these conversations and forming a fertility preservation plan. #cctgynecology #gynocancer #cancerfertility #cdc #dcpc |  |
| Topic: Vulvar cancer awareness for ages 60+ The older a patient gets, the higher their risk of developing vulvar cancer. In fact, more than half of invasive vulvar cancer cases occur in patients older than 70 years old. Remind patients to look for these precancerous/cancerous symptoms when conducting self-checks. #cctgynecology #gynocancer #vulvarcancer #cdc #dcpc |  |
| Topic: Behavioral health resources for gynecologic cancer survivors Gynecologic cancer treatments don’t just take a toll on the body. They can also affect a person’s mental and emotional health and their ability to cope. Patients who are currently receiving treatment can join CancerCare.org’s free, 15-week patient support group. https://bit.ly/3n5D4Uw #cctgynecology #gynocancer #cdc #dcpc |  |
| Topic: Encouraging smoking cessation + providing cessation resources/strategies for low-SES patients While patients might understand the link between smoking and gynecologic cancer, quitting isn’t easy. Use these CDC-recommended interventions to help patients with smoking cessation through counseling, medication, and more. https://bit.ly/3L64ZMe #cctgynecology #gynocancer #quitsmoking #cdc #dcpc |  |
Download All Messages and Graphics How to Post on Social Media
How to Post on Social Media
Start by downloading the ZIP file above. Then double click the downloaded file to unzip and open the folder. Inside, you’ll find three CSV files.
- Messaging.csv contains captions for all messages in the toolkit, organized by topic.
- Bulk – Instagram.csv contains captions for all Instagram messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk – LinkedIn-Facebook-Twitter.csv contains captions for all LinkedIn, Facebook, and Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
Inside the main folder, you’ll also see two sub-folders containing the messaging graphics for all major platforms. The first folder contains rectangular images suited for use on Facebook, Twitter, and LinkedIn. The second folder contains square images suited for Instagram.
Select your platform below for additional instructions.
Gynecological Cancer Resources
| Resource | Description |
|---|---|
| Foundation for Women’s Cancer | Providing education and increasing awareness about gynecologic cancer risk, prevention, early detection and treatment. |
| CancerCare Gynecological Cancers Patient Support Group | A free, 15-week support group for patients living with gynecological cancer who are currently in treatment. |
| Latinas Contras Cancer | An organization providing cancer education, patient navigation, and survivorship services for Latinos in Spanish and English. |
| SaveMyFertility | A resource for adult cancer patients and the parents of children with cancer who want to learn more about preserving their fertility before and during cancer treatment, as well as protecting their hormonal health after treatment. |
| Alliance for Fertility Preservation | Increasing access to information and resources regarding fertility preservation for cancer patients and healthcare professionals. |
| Resolve | Providing financial resources for family building. May be helpful for patients facing infertility and/or those who have the option of fertility preservation before cancer treatment. |
| FORCE | Improve the lives of individuals and families facing hereditary cancer through education, advocacy, and research. |
| National Ovarian Cancer Coalition | Supporting survivors of ovarian cancer and their caregivers, and funding research to advance treatment and find a cure. |
| The National Cervical Cancer Coalition | Helping women, family members and caregivers battle the personal issues related to cervical cancer and HPV and advocating for cervical health in all women. |
| Cervical Cancer Awareness Month Campaign | This cervical cancer awareness month campaign can help your organization implement evidence-based practices when communicating about cervical cancer. |
| Gay and Lesbian Medical Association | A group dedicated to ensuring health equity for LGBTQ+ people through research, advocacy, and education. GLMA also shares resources for both patients and providers caring for LGBTQ+ people. |
| Prevention and Early Diagnosis of Ovarian Cancer and/or Uterine Cancer (e-modules) | A group dedicated to ensuring health equity for LGBTQ+ people through research, advocacy, and education. GLMA also shares resources for both patients and providers caring for LGBTQ+ people. |
*New* HPV Screening At-Home Message Set
In light of the recent FDA approval and availability of the at-home self-sampling HPV screening option, the GW Cancer Center developed timely messaging if your program needs to provide clarity and encouragement for this new option. You can download this entire message and graphics set as you need. Here is the recent news article about this decision, the ASCO article about this decision and the JAMA article about the study.
Files for X (Twitter), Facebook and LinkedIn
Files for Instagram
| Message | Graphic |
| Testing for HPV is getting easier. A new at-home HPV screening kit is FDA-approved and designed for privacy and convenience. It will be available by prescription, through a telehealth service, for people with a cervix who are 25-65 years old, and of average risk. Learn more at: https://nbcnews.to/4jiHY7P |  |
| Soon you can test for HPV from the comfort of your own home! It’s private, easy, and a step toward preventing cervical cancer. Read more about it! https://nbcnews.to/4jiHY7P | 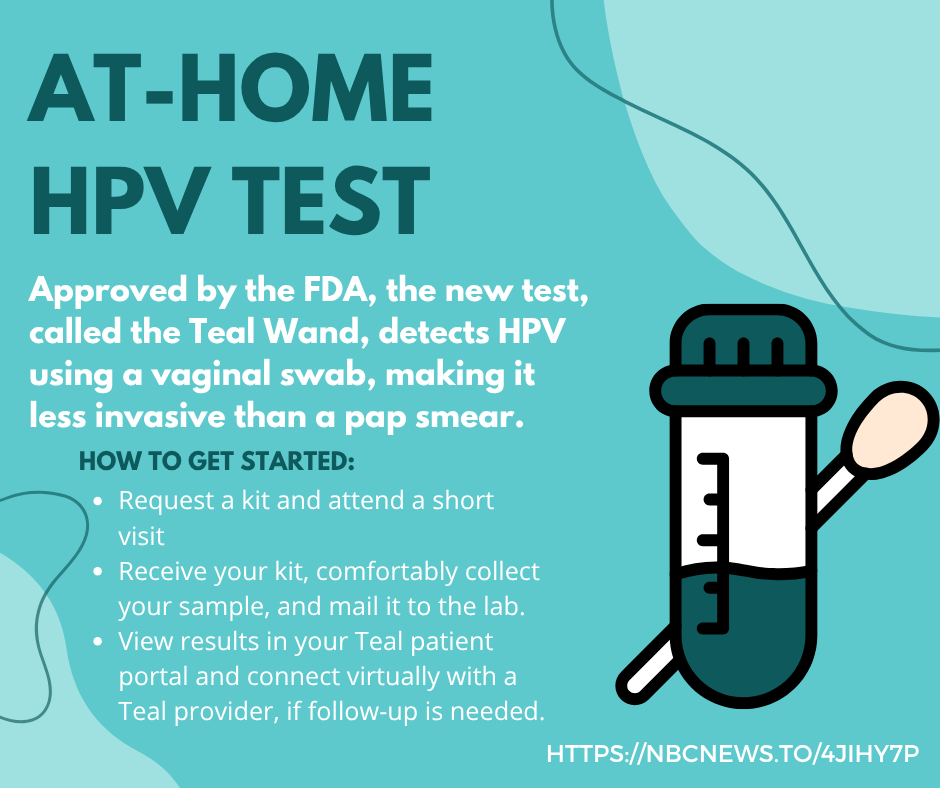 |
| Taking charge of your health has never been easier. With at-home HPV tests, you can screen privately and conveniently. Detecting high-risk HPV early can make all the difference. |  |
| Did you know that most cervical cancers are preventable? With at-home HPV tests, you can screen privately and conveniently. No clinic visit required. Detecting high-risk HPV early can make all the difference. Whether you’re overdue for a Pap test or prefer the comfort of home, self-collection is a proven, FDA-approved option and can be a game-changer in early detection. |  |
| The FDA has recently approved an at-home HPV test! The new test, called the Teal Wand, detects HPV using a vaginal swab, making it less invasive than a pap smear. Read more: https://nbcnews.to/4jiHY7P |  |
| The FDA has recently approved an at-home HPV test! The new test, called the Teal Wand, detects HPV using a vaginal swab, making it less invasive than a pap smear. Read more at: https://nbcnews.to/4jiHY7P |  |
References
- Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/cancer/gynecologic/basic_info/what-is-gynecologic-cancer.htm. Updated August 30, 2022. Accessed March 28, 2023.
- U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2021 submission data (1999-2019): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; https://www.cdc.gov/cancer/dataviz, released in November 2022.
- National Cancer Institute. Uterine cancer—Patient version. https://www.cancer.gov/types/uterine. Accessed March 28, 2023.
- Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/cancer/ovarian/index.htm. Updated August 31, 2022. Accessed March 28, 2023.
- SEER. Cancer of the Vulva – Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/vulva.html
- Musa J, Achenbach CJ, Linda CO, Evans CT, McHugh M, Hou, L, et al. Effect of cervical cancer education and provider recommendation for screening on screening rates: A systematic review and meta-analysis. PLoS One. 2017; 12(12). http://dx.doi.org/10.1371/journal.pone.0183924.
- Ovarian Cancer Research Highlights | Ovarian Cancer News. www.cancer.org. https://www.cancer.org/research/acs-research-highlights/ovarian-cancer-research-highlights.html
- Centers for Disease Control and Prevention. Lynch Syndrome | CDC. www.cdc.gov. Published January 16, 2020. https://www.cdc.gov/genomics/disease/colorectal_cancer/lynch.htm
- Centers for Disease Control and Prevention. Preventing HPV-Associated Cancers. https://www.cdc.gov/cancer/hpv/basic_info/prevention.htm. Updated August 22, 2018. Accessed March 28, 2023.
- Gilkey M, Malo T, Shah P, Hall M, Brewer N. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015; 24(11):1673-1679. http://doi.org/10.1158/1055-9965.EPI-15-0326.
- Fontenot HB, Kornides ML, McRee AL, Gilkey MB. Importance of a team approach to recommending the human papillomavirus vaccination. Journal of the American Association of Nurse Practitioners. 2018;30(7):368-372. doi:https://doi.org/10.1097/jxx.0000000000000064
- Centers for Disease Control and Prevention. What Are the Risk Factors for Ovarian Cancer? https://www.cdc.gov/cancer/ovarian/basic_info/risk_factors.htm. Updated August 31, 2022. Accessed March 28, 2023.
- American Cancer Society. Can Vaginal Cancer Be Prevented? https://www.cancer.org/cancer/vaginal-cancer/causes-risks-prevention/prevention.html. Updated July 21, 2020. Accessed March 28, 2023.
- Henley SJ, Miller JW, Dowling NF, Benard VB, Richardson LC. Uterine cancer incidence and mortality – United States, 1999-2016. MMWR Morb Mortal Wkly Rep. 2018; 67(48):1333–1338. https://doi.org/10.15585/mmwr.mm6748a1.
- Feng Y. The association between obesity and gynecological cancer. Gynecol Minim Invasive Ther. 2015; 4(4):102–105. https://doi.org/10.1016/j.gmit.2015.03.003.
- de Rooij BH, Thomas TH, Post KE, et al. Survivorship care planning in gynecologic oncology-perspectives from patients, caregivers, and health care providers. J Cancer Surviv. 2018;12(6):762-774. doi:10.1007/s11764-018-0713-9
- Jorge S, Masshoor S, Gray HJ, Swisher EM, Doll KM. Participation of Patients With Limited English Proficiency in Gynecologic Oncology Clinical Trials. J Natl Compr Canc Netw. 2023;21(1):27-32.e2. doi:10.6004/jnccn.2022.7068
- Awad E, Paladugu R, Jones N, et al. Minority participation in phase 1 gynecologic oncology clinical trials: Three decades of inequity. Gynecologic Oncology. 2020;157(3):729-732. doi:https://doi.org/10.1016/j.ygyno.2020.03.002
- White-Means SI, Osmani AR. Racial and Ethnic Disparities in Patient-Provider Communication With Breast Cancer Patients: Evidence From 2011 MEPS and Experiences With Cancer Supplement. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2017;54. doi:10.1177/0046958017727104
- Cancer – The Office of Minority Health. Hhs.gov. Published 2019. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=61
- Bruegl AS, Joshi S, Batman S, Weisenberger M, Munro E, Becker T. Gynecologic cancer incidence and mortality among American Indian/Alaska Native women in the Pacific Northwest, 1996-2016. Gynecol Oncol. 2020;157(3):686-692. doi:10.1016/j.ygyno.2020.03.033
- Witte, Catherine; Begay, Tamana D.; and Coe, Kathryn (2010) “Spiritual Care within Oncology Care: Development of a Spiritual Care Program at an Indian Health Service Hospital,” Journal of Health Disparities Research and Practice: Vol. 4: Iss. 3, Article 7.
- Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A Systematic Review of the Discrimination Against Sexual and Gender Minority in Health Care Settings. International Journal of Health Services. 2020;50(1):44-61. doi:10.1177/0020731419885093
- Cook SC, Gunter KE, Lopez FY. Establishing effective health care partnerships with sexual and gender minority patients: recommendations for obstetrician gynecologists. Semin Reprod Med. 2017; 35(05):397-407. https://doi.org/10.1055/s-0037-1604464.
- National LGBT Cancer Network Cultural Competency Training. cancer-network.org. Accessed May 22, 2023. https://cancer-network.org/cultural-competency-training/.
- Stenzel AE, Moysich KB, Ferrando CA, Starbuck KD. Clinical needs for transgender men in the gynecologic oncology setting. Gynecol Oncol. 2020;159(3):899-905. doi:10.1016/j.ygyno.2020.09.038
- Hoover DS, Spears CA, Vidrine DJ, Walker JL, Shih YCT, Wetter DW. Smoking Cessation Treatment Needs of Low SES Cervical Cancer Survivors. American Journal of Health Behavior. 2019;43(3):606-620. doi:https://doi.org/10.5993/ajhb.43.3.14
- Centers for Disease Control and Prevention (2021). HPV Vaccine Recommendations. https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html. Updated November 16, 2021. Accessed March 28, 2023.
- Weeks K, Lynch CF, West M, et al. Rural disparities in surgical care from gynecologic oncologists among Midwestern ovarian cancer patients. Gynecologic Oncology. 2021;160(2):477-484. doi:https://doi.org/10.1016/j.ygyno.2020.11.006

