Human Papillomavirus (HPV) & Prevention
Human papillomavirus, or HPV, is a common virus that is spread through intimate contact.1 Of the approximately 150 types of HPV currently identified, at least 40 occur in the genital area.2 HPV infections are extremely common, and most people will get HPV in their lifetime.2 Many HPV infections are asymptomatic and resolve on their own,2 but some persistent infections can cause cancers of the cervix, vagina, vulva, penis, anus, and throat.1 HPV is also responsible for a substantial portion of anogenital warts in the United States.2
HPV vaccines can prevent both anogenital warts2 and 90% of cancers caused by HPV.3 Vaccination is recommended for all adolescents and young adults through age 26, with a first dose administered as early as age nine and a second dose administered six months later.3 Individuals who did not receive their first dose until after their 15th birthday should receive three doses given over six months.3 People ages 26-46 years old can discuss with their provider the risk of new HPV infections and if they would benefit from HPV vaccination.3
This health awareness social media toolkit can help your cancer control organizations implement evidence-based practices when communicating about HPV prevention.
Data and Statistics
More than 42 million people in the United States have a form of HPV that can cause other diseases, and 13 million Americans get HPV every year.1 HPV causes approximately 36,000 new cancer cases in the United States annually.1 Since the development of HPV vaccines, the rate of infections of HPV types that cause genital warts or cancer has dropped by 88% among teen girls and by 81% among young adult women.4 Among vaccinated women, incidences of cervical precancers caused by HPV types most commonly linked to cervical cancer have dropped by 40 percent.4 To date, more than 135 million doses of HPV vaccines have been administered in the United States.5
Best Practices for Communicating About HPV Prevention
Communicating with Diverse Audiences
Communication-related issues may also play a role in cancer disparities.13 Consider the information most useful to each diverse group (see below for specific messaging and read more on health disparities here). Tailor communication to these populations of focus with messages that also address conditions where these communities live, learn, work and play, as these social determinants of health can impact a wide range of health risks and outcomes. To ensure messages resonate with the coalition’s intended audience, we also recommend referring to the National Networks’ existing resources and adapting messages to reflect individuals with lived experiences.
HPV Messages and Graphics
Download All Messages and Graphics How to Post on Social Media
| Topics | Suggested Images |
|---|---|
| Topic: Share the benefits of HPV vaccination Getting the #HPV vaccine is in every individual’s best interest. Share these fast facts to help patients understand the benefits of getting the HPV vaccine. #ccthpv #cdc #dcpc |  |
| Topic: Provide age-based recommendations for HPV vaccination When should you start recommending the #HPV vaccine to your patients? Help individuals manage their vaccination schedule by sharing these age-based @CDC_Cancer guidelines. #ccthpv #cdc #dcpc |  |
| Topic: Emphasize the importance of follow-up recommendations Did a parent refuse your recommendation to administer the #HPV vaccine to their child? Don’t give up! Studies show that persistent recommendations can change a parent’s mind and increase the rate of HPV vaccinations among adolescents. #ccthpv #cdc #dcpc |  |
| Topic: Helping providers talk with parents about HPV vaccines Talking about the #HPV vaccine with parents is vital to reducing the risks of certain cancers for children. However, these conversations aren’t always easy for providers to navigate. Use these @CDC_Cancer tactics to improve how you recommend HPV vaccination. #ccthpv #cdc #dcpc |  |
| Topic: Provide HPV informational resources that providers can share with transgender men Transmasculine patients may have questions on navigating conversations about #HPV with providers. Review and share this resource from the @FenwayHealth to help them prepare for this discussion. https://tinyurl.com/52fx3nd9 #ccthpv #cdc #dcpc #transhealth |  |
| Topic: Tips for talking to parents about HPV vaccines Providers, if you need help navigating conversations about #HPV vaccines with parents of adolescents and young adults, this @CDC_Cancer guide can help you answer some of the most commonly asked parent questions. https://bit.ly/40ACiwD #ccthpv #cdc #dcpc |  |
| Topic: Resources for providers to share with parents Having informational material ready can help providers communicate the importance of timely #HPV vaccinations. Share these @CDC_Cancer resources within your networks, including fact sheets on HPV and vaccine safety, schedules, and follow-up letters they can share with parents. https://tinyurl.com/2p943h48 #ccthpv #cdc #dcpc |  |
| Topic: Provide parents with informational resources about potential side effects of the vaccine Acknowledging possible side effects of #HPV vaccines could help to establish trust with your patients and their parents. Share this @CDC_Cancer HPV vaccine safety document with your patients to inform them of potential side effects. https://tinyurl.com/5d864c45 #ccthpv #cdc #dcpc |  |
| Topic: Remind providers about the importance of HPV vaccinations for men Only 10% of cisgender men between the ages of 18-26 report receiving the #HPV vaccine, compared to 42% of cisgender women. The HPV vaccine can protect against genital warts, anal cancer, and penile cancer, in addition to preventing HPV transmission to sex partners. Make sure to recommend the vaccine to all patients regardless of gender. #ccthpv #cdc #dcpc |  |
| Topic: Reinforce the relationship between HPV and cervical cancer when recommending vaccinations to Black patients Research reveals that 36% of Black women don’t know that #HPV can cause #cervicalcancer due to differences in how Black women learn and/or communicate about HPV and cervical cancer. Start the discussion early and share the benefits of HPV vaccination with these individuals. #ccthpv #cdc #dcpc #blackhealth |  |
| Topic: Tips for caring for LGBTQ+ patients Caring for LGBTQI+ patients require knowing how to communicate respectfully and making them feel at ease. When having conversations about #HPV, remember these strategies from @cancerLGBT for creating a welcoming environment. #cdc #dcpc #ccthpv #lgbthealth |  |
| Topic: Tips for caring for transgender patients How you communicate with transgender patients about #HPV could play a critical role in whether they begin and finish HPV vaccination, as hormone therapy and gender-affirming surgeries may or may not affect HPV detection. Consider these recommendations for transgender inclusivity from @cancerLGBT. https://tinyurl.com/4hkjuypz #cdc #dcpc #ccthpv #transhealth |  |
| Topic: Encourage cervical cancer screenings for transmasculine patients #Transmasculine patients with a cervix still need to be screened for cervical cancer. Check out the emerging research on #self-sampling for #trangender men and #rural cisgender women. https://tinyurl.com/4t4amutn& https://tinyurl.com/4j5rx3zh #ccthpv #cdc #dcpc |  |
| Topic: Acknowledge lower vaccination rates among AANHPI patients Data reveals that Asian American individuals (not including Native Hawaiians and Pacific Islanders) have the lowest rates of #HPV vaccination. Share information and resources on HPV vaccination for this community. #ccthpv #cdc #dcpc #asianamericanhealth |  |
| Topic: Provide Spanish-language resources to increase HPV vaccination coverage among Hispanic/Latino/a/x patients #DidYouKnow that #HPV vaccination rates are higher among Hispanic and Latin/o/a/x adolescents when Spanish-language information and resources are available to their parents? @ImmunizeOrg provides a Spanish-language translation of @CDC_Cancer’s HPV fact sheet that you can provide to patients. Translations are also available in French, Chinese, Arabic, and more. https://tinyurl.com/3tkf7mht #ccthpv #cdc #dcpc |  |
| Topic: Recommend HPV vaccination as a form of cervical cancer prevention among AI/AN patients Even though American Indian/Alaska Native youth aged 13-17 have higher rates of #HPV vaccination compared to White youth, they still experience a higher incidence of cervical cancer. To combat this, share information about how the HPV vaccine can prevent cervical cancer in this population. #ccthpv #cdc #dcpc #aianhealth |  |
| Topic: Policy, Systems and Environmental (PSE) Change Consider using multi-media campaigns to increase #HPV vaccination rates in your state. Discover how @MichiganCancer increased HPV vaccination rates in their Hispanic population by developing a multimedia campaign with Spanish-language HPV public service announcements and educational materials: https://tinyurl.com/yc28ab37 #ccthpv #cdc #dcpc #PSEchange |  |
| Topic: Policy, Systems and Environmental (PSE) Change Within @DartmouthCancer’s catchment areas of New Hampshire and Vermont, #HPV vaccination rates are much higher than in other parts of the U.S., but rates have plateaued over time. Learn how these two states conducted an environmental scan to understand the barriers and facilitators of HPV vaccination and how these findings support their states’ collaborative interventions: https://tinyurl.com/5n6k26sx #ccthpv #cdc #dcpc #PSEchange |  |
| Topic: Using recall/reminder activities to boost vaccination rates Reminder and recall systems are effective for both your costs and your patients! Research shows that activities like personal phone calls, text messages, postcards, and more can boost #vaccination rates. Try using these recall/reminder resources from the American Academy of Pediatrics to encourage HPV vaccinations in your area. https://tinyurl.com/ftj56fpy |  |
Download All Messages and Graphics How to Post on Social Media
How to Post on Social Media
Start by downloading the ZIP file above. Then double click the downloaded file to unzip and open the folder. Inside, you’ll find three CSV files.
- Messaging.csv contains captions for all messages in the toolkit, organized by topic.
- Bulk – Instagram.csv contains captions for all Instagram messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk – LinkedIn-Facebook.csv contains captions for all LinkedIn, Facebook, and Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk – Twitter.csv contains captions for all Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
Inside the main folder, you’ll also see two sub-folders containing the messaging graphics for all major platforms. The first folder contains rectangular images suited for use on Facebook, Twitter, and LinkedIn. The second folder contains square images suited for Instagram.
Select your platform below for additional instructions.
HPV Resources
| Resource | Description |
|---|---|
| Equality California’s Diversity, Equity, and Inclusion Program | A free, online LGBTQ+ HPV training, “Increasing Vaccination Rates for the LGBTQ+ Community.” This curriculum outlines evidence-based, LGBTQ+ sensitive strategies for increasing HPV vaccination rates among adolescents. Training engages and trains healthcare workers in evidence-based, LGBTQ+ sensitive practices to encourage HPV vaccination, and to increase HPV vaccination rates among LGBTQ+ populations, particularly transgender and gender-nonconforming youth. |
| Gay and Lesbian Medical Association | A group dedicated to ensuring health equity for LGBTQ+ people through research, advocacy, and education. GLMA also shares resources for both patients and providers caring for LGBTQ+ people. |
| HPV Cancers Alliance | Sharing education and resources to increase HPV vaccination rates and prevent HPV-related cancers. |
| HPV Information for Parents | CDC education on HPV, vaccines, and HPV risks to encourage parents to give their children the HPV vaccine. |
| HPV Resources for Professionals | CDC tools and guides healthcare professionals can use to communicate accurate information with their staff members and the parents of adolescent and young adult patients. |
| “HPV Vaccination” Cancer Plan Tip Sheet | Tip sheet used to help CCC program staff, coalition staff, and volunteers update their CCC plans. The Tip Sheet includes tips about engaging partners, identifying and using the right data, setting baselines and targets, and crafting objectives and strategies, as well as a list of practical questions to guide discussion on the topic with your coalition. |
| Immunize.org Vaccine Information Statements | Providing CDC curated HPV Vaccine Information Statements in English and 33 other languages. |
| Make it Your Own | A tool for helping medical professionals to create tailored health communications with evidence-based messaging and customized images. |
| The National Cervical Cancer Coalition | Helping women, family members and caregivers battle the personal issues related to cervical cancer and HPV and advocating for cervical health in all women. |
| National LGBT Cancer Network | Improving the lives of LGBTQ+ cancer survivors through advocacy, education, and training. |
| NOMAN Campaign | A campaign aiming to increase HPV vaccination rates for all genders, promote parent education, and influence policy related to HPV vaccinations. |
| Pap-a-thon Toolkit | Hosting a Women’s Community Health Event – Increasing Cervical Cancer Screening in Rural Tribal Communities (itcmi.org) |
| Path to a Bright Future: HPV Cancer Prevention | Addresses opportunities for HPV prevention, HPV vaccination and increasing vaccination coverage, and the St. Jude HPV cancer prevention program (use passcode C2NTM*&v to access) |
| Queer Health is Power Social Media National Partner Packet | A new set of social media shareables focused on access to care, LGBTQ+ screening, and HPV. This project was piloted in New York and is now available for national use. |
*New* HPV Screening At-Home Message Set
In light of the recent FDA approval and availability of the at-home self-sampling HPV screening option, the GW Cancer Center developed timely messaging if your program needs to provide clarity and encouragement for this new option. You can download this entire message and graphics set as you need. Here is the recent news article about this decision, the ASCO article about this decision and the JAMA article about the study.
Files for X (Twitter), Facebook and LinkedIn
Files for Instagram
| Message | Graphic |
| Testing for HPV is getting easier. A new at-home HPV screening kit is FDA-approved and designed for privacy and convenience. It will be available by prescription, through a telehealth service, for people with a cervix who are 25-65 years old, and of average risk. Learn more at: https://nbcnews.to/4jiHY7P |  |
| Soon you can test for HPV from the comfort of your own home! It’s private, easy, and a step toward preventing cervical cancer. Read more about it! https://nbcnews.to/4jiHY7P | 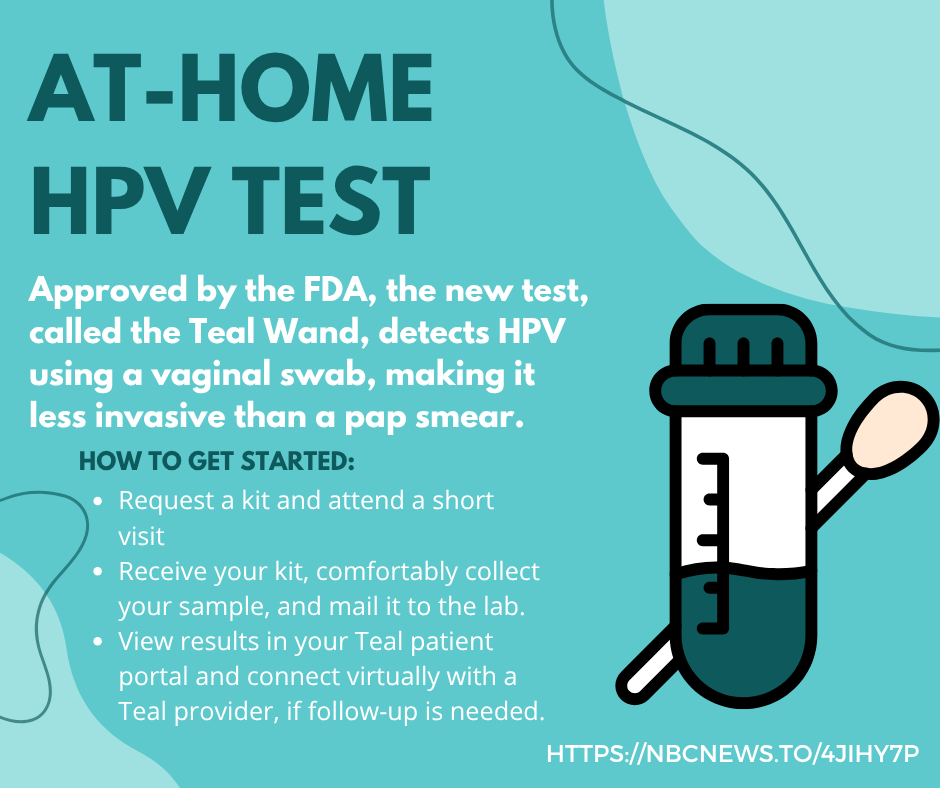 |
| Taking charge of your health has never been easier. With at-home HPV tests, you can screen privately and conveniently. Detecting high-risk HPV early can make all the difference. |  |
| Did you know that most cervical cancers are preventable? With at-home HPV tests, you can screen privately and conveniently. No clinic visit required. Detecting high-risk HPV early can make all the difference. Whether you’re overdue for a Pap test or prefer the comfort of home, self-collection is a proven, FDA-approved option and can be a game-changer in early detection. |  |
| The FDA has recently approved an at-home HPV test! The new test, called the Teal Wand, detects HPV using a vaginal swab, making it less invasive than a pap smear. Read more: https://nbcnews.to/4jiHY7P |  |
| The FDA has recently approved an at-home HPV test! The new test, called the Teal Wand, detects HPV using a vaginal swab, making it less invasive than a pap smear. Read more at: https://nbcnews.to/4jiHY7P |  |
References
- Centers for Disease Control and Prevention. HPV vaccine protects against HPV and the cancers it causes. Centers for Disease Control and Prevention. Published August 22, 2019. https://www.cdc.gov/hpv/parents/about-hpv.html
- CDC. Human Papillomavirus (HPV) Infection – STI Treatment Guidelines. www.cdc.gov. Published July 14, 2021. https://www.cdc.gov/std/treatment-guidelines/hpv.htm
- CDC. Cancers Caused by HPV Are Preventable. Published 2019. https://www.cdc.gov/hpv/hcp/protecting-patients.html
- CDC. Vaccine for HPV. Published 2019. www.cdc.gov/hpv/parents/vaccine-for-hpv.html
- CDC. HPV Vaccine Safety. Centers for Disease Control and Prevention. Published November 25, 2019. https://www.cdc.gov/hpv/hcp/vaccine-safety-data.html
- CDC. HCP | Vaccine Administration | Educate Parent or Patient | CDC. www.cdc.gov. Published September 25, 2019. https://www.cdc.gov/vaccines/hcp/admin/educating-patients.html
- Ylitalo KR, Lee H, Mehta NK. Health Care Provider Recommendation, Human Papillomavirus Vaccination, and Race/Ethnicity in the US National Immunization Survey. American Journal of Public Health. 2013;103(1):164-169. doi:https://doi.org/10.2105/ajph.2011.300600
- Reno JE, Thomas J, Pyrzanowski J, et al. Examining strategies for improving healthcare providers’ communication about adolescent HPV vaccination: evaluation of secondary outcomes in a randomized controlled trial. Hum Vaccin Immunother. 2019;15(7-8):1592-1598. doi:10.1080/21645515.2018.1547607
- Lake PW, Kasting ML, Christy SM, Vadaparampil ST. Provider perspectives on multilevel barriers to HPV vaccination. Human Vaccines & Immunotherapeutics. 2019;15(7-8):1784-1793. doi:https://doi.org/10.1080/21645515.2019.1581554
- Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Preventive Medicine. 2013;57(5):414-418. doi:https://doi.org/10.1016/j.ypmed.2013.05.013
- CDC. 5 Ways to Boost Your HPV Vaccination Rates. Published 2019. https://www.cdc.gov/hpv/hcp/boosting-vacc-rates.html
- Gilkey MB, Calo WA, Marciniak MW, Brewer NT. Parents who refuse or delay HPV vaccine: Differences in vaccination behavior, beliefs, and clinical communication preferences. Human Vaccines & Immunotherapeutics. 2016;13(3):680-686. doi:https://doi.org/10.1080/21645515.2016.1247134
- Paez KA, Allen JK, Beach MC, Carson KA, Cooper LA. Physician cultural competence and patient ratings of the patient-physician relationship. J Gen Intern Med. 2009;24(4):495-498. doi:10.1007/s11606-009-0919-7
- Ojeaga A, Alema-Mensah E, Rivers D, Azonobi I, Rivers B. Racial Disparities in HPV-related Knowledge, Attitudes, and Beliefs Among African American and White Women in the USA. J Cancer Educ. 2019;34(1):66-72. doi:10.1007/s13187-017-1268-6
- Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A Systematic Review of the Discrimination Against Sexual and Gender Minority in Health Care Settings. International Journal of Health Services. 2020;50(1):44-61. doi:10.1177/0020731419885093
- Chidobem I, Tian F, Ogbuokiri E, et al. Trends in HPV and HPV Vaccine Awareness among Gay and Bisexual Males in the U.S. Vaccines (Basel). 2022;10(4):604. Published 2022 Apr 13. doi:10.3390/vaccines10040604
- Singh V, Gratzer B, Gorbach PM, et al. Transgender Women Have Higher Human Papillomavirus Prevalence Than Men Who Have Sex With Men-Two U.S. Cities, 2012-2014. Sex Transm Dis. 2019;46(10):657-662. doi:10.1097/OLQ.0000000000001051
- Stewart T, Lee YA, Damiano EA. Do Transgender and Gender Diverse Individuals Receive Adequate Gynecologic Care? An Analysis of a Rural Academic Center. Transgender Health. Published online January 22, 2020. doi:https://doi.org/10.1089/trgh.2019.0037
- Smith J. HPV Self-Collection Kits Increase Screening Among Under-screened, Under-served Women in North Carolina. Newsroom. Published May 12, 2023. Accessed September 20, 2023. https://news.unchealthcare.org/2023/05/hpv-self-collection-kits-increase-screening-among-under-screened-under-served-wo…
- Dhillon N, Oliffe JL, Kelly MT, Krist J. Bridging Barriers to Cervical Cancer Screening in Transgender Men: A Scoping Review. American Journal of Men’s Health. 2020;14(3):155798832092569. doi:https://doi.org/10.1177/1557988320925691
- McElfish PA, Narcisse MR, Felix HC, et al. Race, Nativity, and Sex Disparities in Human Papillomavirus Vaccination Among Young Adults in the USA. J Racial Ethn Health Disparities. 2021;8(5):1260-1266. doi:10.1007/s40615-020-00886-5
- Reiter PL, Pennell ML, Martinez GA, Perkins RB, Katz ML. HPV vaccine coverage across Hispanic/Latinx subgroups in the United States. Cancer Causes Control. 2020;31(10):905-914. doi:10.1007/s10552-020-01331-y
- Zhao R, Prizment AE, Shalini Kulasingam. Lower human papillomavirus vaccine initiation and completion among Asian American adolescents compared to their peers: National Health and Nutritional Examination Survey 2011–2018. Cancer Causes & Control. Published online March 27, 2023. doi:https://doi.org/10.1007/s10552-023-01685-z
- Pingali C. Vaccination Coverage Among Adolescents Aged 13–17 Years — National Immunization Survey–Teen, United States, 2022. MMWR Morbidity and Mortality Weekly Report. 2023;72. doi:https://doi.org/10.15585/mmwr.mm7234a3
- Bruegl AS, Joshi S, Batman S, Weisenberger M, Munro E, Becker T. Gynecologic cancer incidence and mortality among American Indian/Alaska Native women in the Pacific Northwest, 1996-2016. Gynecol Oncol. 2020;157(3):686-692. doi:10.1016/j.ygyno.2020.03.033
- U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2022 submission data (1999-2020): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; https://www.cdc.gov/cancer/dataviz, released in June 2023.

