About the Lung Cancer Awareness Toolkit
We would like to acknowledge and thank our co-branding partners for their contributions to this project:
November is Lung Cancer Awareness Month. According to the Centers for Disease Control and Prevention (CDC), “more people in the United States die from lung cancer than any other type of cancer.”[1] Lung cancer screening recommendation has evolved over the past 10 years and messaging is needed to increase normalcy of routine lung cancer screenings, in addition to continued messaging on avoiding commercial tobacco and radon mitigation. Although the number of screening facilities in the United States has increased, screening uptake has been slow.
Data and Statistics
In 2021, the latest year comprehensive incidence data are available, 209,500 new lung cancers were reported in the U.S., and in 2022, 131,888 people died from lung cancer[2]. In 2021, for every 100,000 people, 49 new lung and bronchus cancer cases were reported.[3] For every 100,000 people, 30 people died of lung and bronchus cancer in 2022—the highest death rate of cancers in the U.S.[4] Because of health service disruptions throughout 2020 and 2021 due to the COVID-19 pandemic, cancer screening, diagnosis, and central cancer registry reporting may be delayed and artificially reduced.
Lung cancer incidence and mortality rates vary by region, states and within states. Lung cancer affects people from all backgrounds. Use the National Cancer Institute’s State Cancer Profiles interactive tool to customize messages to align communications with geographic location data for populations who experience disproportionate burdens and needs related to lung cancer.[5]
Screening with annual low-dose CT scans can reduce the lung cancer death rate by up to 20% by detecting tumors at early stages when the cancer is more likely to be curable. Lung cancer screening has saved 80,000 additional years of life, leading to $40 million in savings, which would increase to 500,000 additional years of life and $500 million in savings if all those eligible had been screened.[6] For screening to be most effective, more high-risk people should be screened annually—currently screening rates remain low among those at high risk. Nationally, only 18% of eligible individuals are up to date with their lung cancer screening.[7]
| *Note about terminology: Here we report statistics the way in which they are reported in our source references, while emphasizing their limitations. Data are currently reported as binary sex data (male or female) and ignore gender and sex characteristic differences that make up the intersex spectrum, making it difficult to explain differences across gender and sexual orientations. While the latest North American Association of Central Cancer Registries (NAACCR) data dictionary includes multiple options beyond sex variables, the field may be underused or underreported. We advocate for systematic collection of sex assigned at birth, gender identity, sexual orientation, and intersex status to inform and advance evidence-based guidelines. We use gender-neutral language when possible. Until better data are available, it is reasonable to assume sex and gender are conflated in most data sources. |
Best Practices for Communicating About Lung Cancer
Promote patient-healthcare team discussions of lung cancer risk
- Lung cancer risk factors include smoking, secondhand smoke exposure, radon, and other environmental exposures (e.g. asbestos, pollution).[8] Advocate for comprehensive smoke-free air policies, radon mitigation, and workplace protections to mitigate exposures.
- Health care professionals should use every opportunity to educate and ask patients in a culturally appropriate way about their smoking history and determine if someone meets the eligibility criteria for screening.
- Familial history of lung or other cancers may increase risk for lung cancer.[9] Encourage patients to discuss family history with their primary care doctor.
- Having a family history of lung cancer is associated with a higher perceived risk of lung cancer among people who currently smoke or used to smoke. This can influence a person’s willingness to pursue lung cancer screening.[10] Provide the public with information about the link between family history and lung cancer risk.
- Radon exposure is the leading cause of lung cancer for people who have never smoked.[11] It is estimated that about 20,000 to 40,000 people who do not smoke get lung cancer each year, with 2,900 cases estimated to be associated with radon.[12] Advocate for radon mitigation, especially in areas where radon is known to be elevated.
Provide information about lung cancer screening and promote screening to people who are recommended to be screened
- The U.S. Preventive Services Task Force (USPSTF) recommends yearly lung cancer screening with low-dose computed tomography (also called a low-dose CT scan, or LDCT) for people who have a 20 pack-year or more smoking history, smoke now or have quit within the past 15 years and are between 50 and 80 years old.[13] Pack-years are the number of packs (20 cigarettes) smoked daily, multiplied by the average number of years smoked. For example, a person could have a 20-pack history if the person smoked 1 pack a day for 20 years or 2 packs a day for 10 years. Encourage people who meet screening eligibility to be screened for lung cancer.
- Provide culturally appropriate information in plain language in recipients’ preferred language.[14]
- Promote adherence to annual screening by reminding individuals of the importance of lung cancer screening.[15] Educating people about lung cancer screening is not a one-time event, but something to be done routinely.
Provide information about long-term care and survivorship issues in addition to treatment information
- Provide survivors of lung cancer with survivorship services and resources, such as tobacco cessation services, physical activity support, weight management support, elimination or moderation of alcohol consumption, appropriate vaccinations, other regular cancer screenings and pain management.[16]
- Promote patient-clinician discussion of palliative care options throughout treatment. [17] The introduction of palliative care early during treatment may prolong survival and improve quality of life for patients with advanced lung cancer.[18]
Remind healthcare professionals about the importance of communication and its effect on patients’ quality of life
- Reduce cancer information overload in your communication strategy by orienting patients and survivors to reliable sources and culturally relevant support aids. [19]
- Promote interpersonal aspects of communication and shared decision-making processes between healthcare professionals and people who could benefit from lung cancer screening.[20]
- Educate clinicians to improve awareness of implicit bias. People who are Black and other marginalized groups continue to face barriers to accessing high quality, patient-centered care, specifically relating to specialty care, medical tests, and patient-clinician communication. [21]
Address and combat stigma often associated with a lung cancer diagnosis
- Stigma is rooted in attributes, characteristics, or behaviors that devalue individuals or groups; it can be perceived or felt, which can result in groups and individuals internalizing guilt or shame. Stigma can negatively impact screening behaviors and increase psychological distress. [22]
- Tailor messages to address stigma and social barriers to lung cancer screening. People who smoke may feel blame or stigma during clinical encounters.[23] Messages should be empathetic and stigma-reducing.
- Normalize lung cancer screening, especially annual lung cancer screening even when initial screens are negative and normal. Pair lung cancer screening education with other cancer screening messages. Remind people that screening supports early detection of multiple cancers, which can optimize survival and health outcomes of those diagnosed at an earlier stage of disease.[24]
- Encourage screening through a ‘gain’ frame rather than ‘loss’ frames to help balance fear of lung cancer screening.[25]
- Don’t wait until it’s too late can be rephrased to: Take action now.
- Stop harming yourself. Stop Smoking can be rephrased to: Start living. Stop Smoking.
- In addition to the physical benefits of quitting smoking, it can also have a positive impact on one’s social life. This can be rephrased to: In addition to the negative physical effects of smoking, it can have a negative impact on one’s social life.
Special Recommendations for Healthcare Professionals
- Clinicians should avoid stigmatizing the illness.[26] Refer to the International Association for the Study of Lung Cancer’s (IASLC) Language Guide for guidelines on best practices. [27]
- Provide high-quality shared decision-making support, which includes leaving time for open-ended questions to patients to increase screening uptake and tobacco cessation.[28]
- Consider alternative risk-based screening methods, like the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial 2012 (PLCOm2012) model, to reduce disparities in lung cancer screenings for people who are Black or from other diverse groups. [29]
- Integrate patient navigators within lung cancer screening programs to increase screening use and adherence. Patient navigators can assist people with barriers to lung cancer screening and have unique relationships with patients to overcome mistrust or fear about getting screening. [30]
- Initiate the discussion on lung cancer screening, describing the benefits and risks of lung cancer screening for eligible people. Don’t assume someone knows what a pack year is or understands eligibility criteria. [31]
- Use CDC planning guides to implement evidence-based interventions to increase lung cancer screenings, including patient reminders, structural barrier reduction, and provider reminders.
- Address the need for shared decision-making for someone before they receive lung cancer screening, including decision aids, information about the importance of adherence to lung cancer screening, and tobacco cessation support.
- Develop and use culturally sensitive shared decision-making aids to reduce inequities in lung cancer screening and adherence. [32]
Communicating with Diverse Audiences
Cancer health disparities are complex and affected by various factors, including social determinants of health, behavior, biology, and genetics.[33] Overlap of these factors, referred to as intersectionality, can lead to many people experiencing multiple forms of marginalization. Tailor information for those who are disproportionately affected by lung cancer.
Lung Cancer Resources
| Resource | Description |
|---|---|
| American Lung Association: Help and Support Resources | A strong support system can improve health outcomes. Connect with these resources offered by the American Lung Association. |
| American College of Radiology | Use the search form to find imaging facilities in your area that are accredited by the American College of Radiology. |
| Are You At Risk for Radon? | The CDC released this video to explain the risks of radon exposure and what people can do to mitigate indoor exposure. |
| Blueprint to Transform a Lung Cancer Screening Program | End Lung Cancer Now developed a plan for organizations building lung cancer screening programs |
| Cancer Data Visualization Tool | The Cancer Statistics Data Visualization tool provides the most up-to-date information from the CDC on lung and other cancers. |
| Caregiver Resource Guide | This guide from the American Cancer Society is a tool for people and families who are caring for someone with cancer. |
| How to Quit Smoking – CDC | This CDC page links to free resources for quitting smoking, including a quitline, text messaging services, and phone app. |
| Clinician Brief: Radon | This brief on radon from the Agency for Toxic Substances & Disease Registry (ATSDR) provides clinical information on radon and its affiliated risks. |
| Comprehensive Cancer Control Webinar Series on Lung Cancer | The American Cancer Society CCC conducted a series of webinars on lung cancer control in 2020. Topics ranged from tobacco cessation to lung cancer screening. |
| E-Cigarettes | While CDC continues to research the effects of e-cigarettes and vapes, it recommends that the best way to reduce risk of negative outcomes is to refrain from using these products. |
| Lung Cancer Screening Resource Sheet from Comprehensive Cancer Control National Partnership (CCCNP) | The Comprehensive Cancer Control National Partnership created a lung cancer screening tip sheet for comprehensive cancer control coalitions. |
| LungCheck tools | LungCheck is a free resource on lung cancer screening developed by New York-Presbyterian and Weill Cornell. It has tools for both patients and clinicians to understand screening and eligibility. |
| LUNGevity | LUNGevity offers an extensive collection of resources for people who have lung cancer and caregivers. |
| Lung Cancer Screening Day | National Lung Cancer Screening Day, on the second Saturday of November, raises awareness of early detection through regular lung cancer screening and aims to reduce access disparities. |
| Lung Cancer Stigma Communications Assessment Tool (LCS-CAT) | From the American Cancer Society and National Lung Cancer Roundtable, this tool helps construct and evaluate lung cancer communication materials. |
| National LGBTQ+ Cancer Network | The National LGBTQ+ Cancer Network offers extensive resources to support patients, clinicians, and caregivers. |
| National Lung Cancer Roundtable (NLCRT) | The National Lung Cancer Round Table (NLCRT) is a national coalition of public, private, and voluntary organizations, and invited individuals, dedicated to reducing the incidence of and mortality from lung cancer in the United States through coordinated leadership, strategic planning, and advocacy. |
| National Native Network: Keep It Sacred | A national network of Tribes, tribal organizations and health programs working to decrease commercial tobacco use and cancer health disparities among American Indian and Alaska Native peoples. The resource offers technical assistance, culturally relevant resources, and a place to share information and lessons learned, as part of a community of tribal and tribal-serving public health programs. |
| State of Lung Cancer, American Lung Association | State of Lung Cancer includes state level lung cancer data on burden and disparities that is easy to use for all audiences. |
| Tobacco Cessation for Cancer Survivors: A Resource Guide for Local Health Departments | This guide from NACCHO describes the role of local health departments in minimizing the impact of cancer in their communities. |
| Tobacco Cessation Tools and Resources | The American Society of Clinical Oncology explains how to incorporate the “5 As” —Ask, Advise, Assess, Assist, and Arrange—for quitting tobacco. |
Lung Cancer Awareness Toolkit Social Media Messages and Graphics
| Message | Suggested Graphic |
|---|---|
November is Lung Cancer Awareness Month. Early detection saves lives. If you’re over 50 and previously or currently smoke, lung cancer screening is recommended for some people who are at high risk! #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| It’s Lung Cancer Awareness Month. Screenings can catch cancer early when it’s more treatable. If you have smoked tobacco and are over 50-years-old, don’t wait. Ask your doctor about lung cancer screening. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screenings can find cancer early, when it’s easier to treat. If you smoke now or smoked tobacco regularly in the past and are at least 50 years old, don’t wait—talk to your doctor about getting screened today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 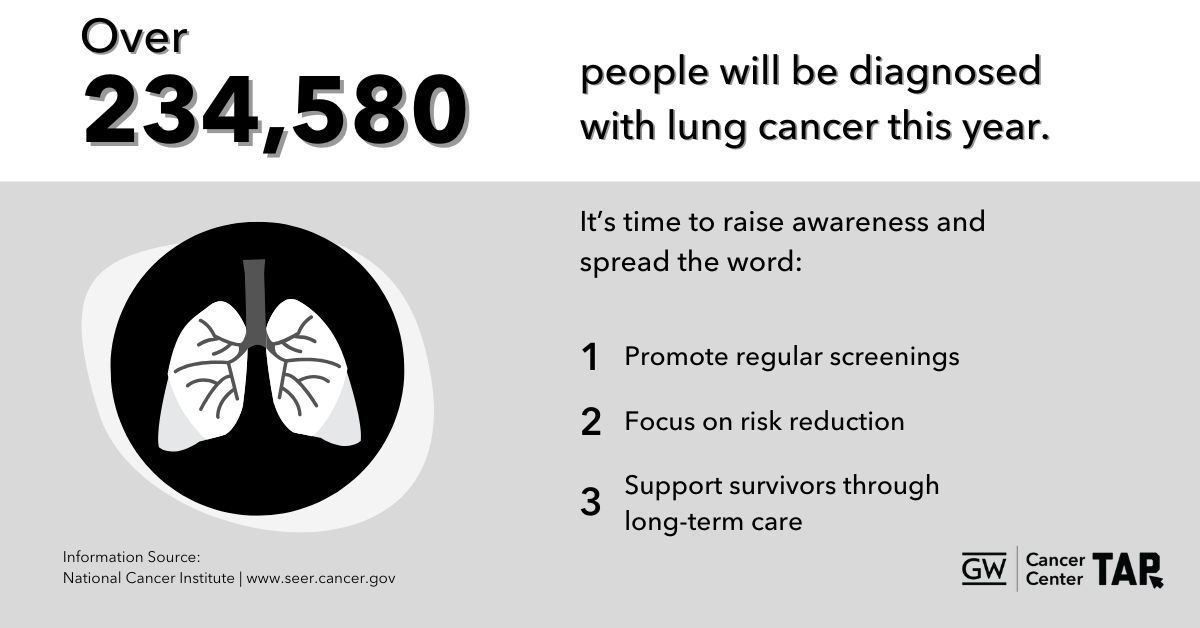 Download Image |
| [November 9th] It’s National Lung Cancer Screening Day! Screening can find lung cancer early, when it’s most treatable. If you are 50 years or older with a history of regular smoking—don’t wait. Get screened today and take control of your health. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| [November 9th] Lung cancer screenings are quick and can make a difference. If your doctor recommends lung screening, they do NOT think you have lung cancer, they’re just checking! Contact your doctor today to learn more. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Did you know? Lung cancer screenings can detect cancer early, when it’s easier to treat. If you are age 50+, don’t wait—talk to your doctor about whether screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 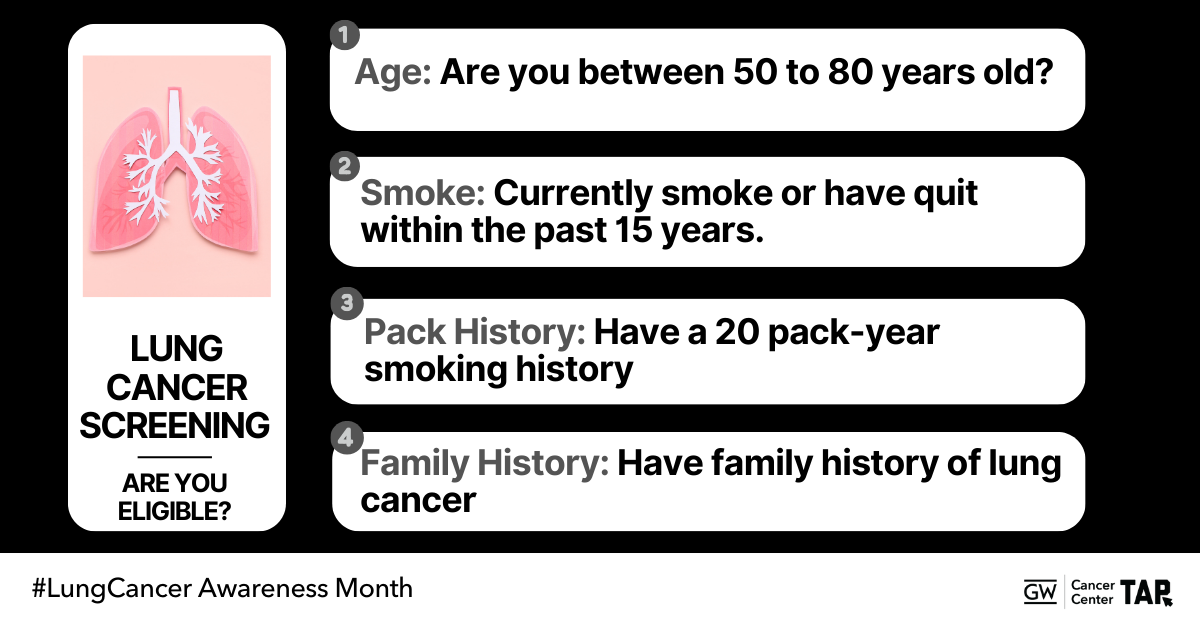 Download Image |
| Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives! #LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 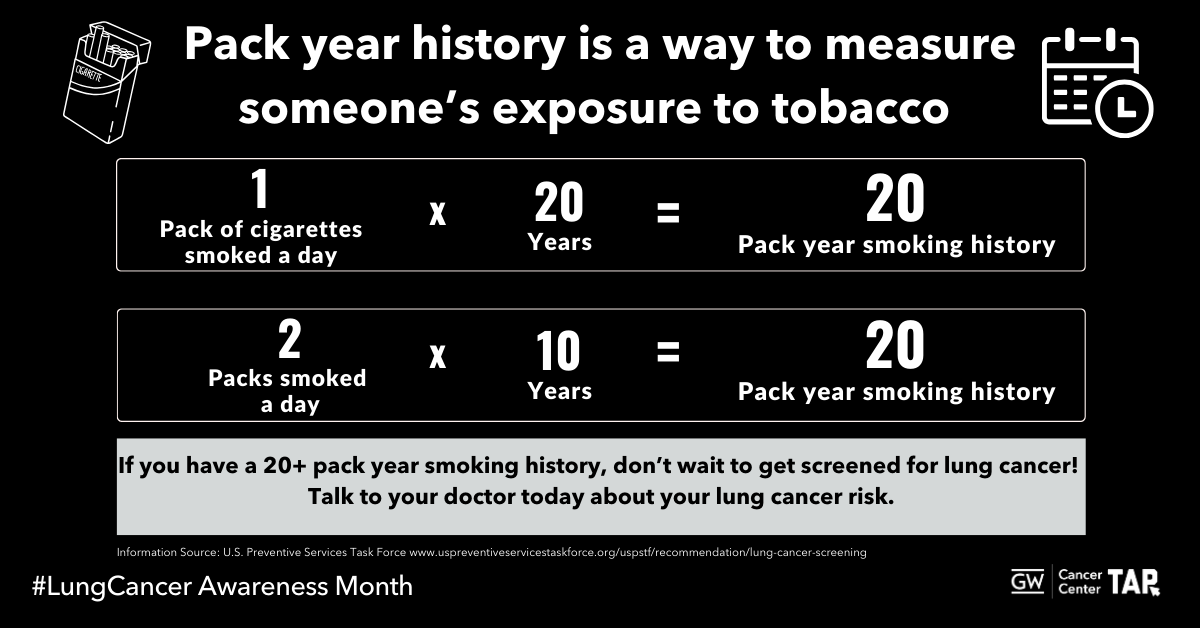 Download Image |
Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives!#LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 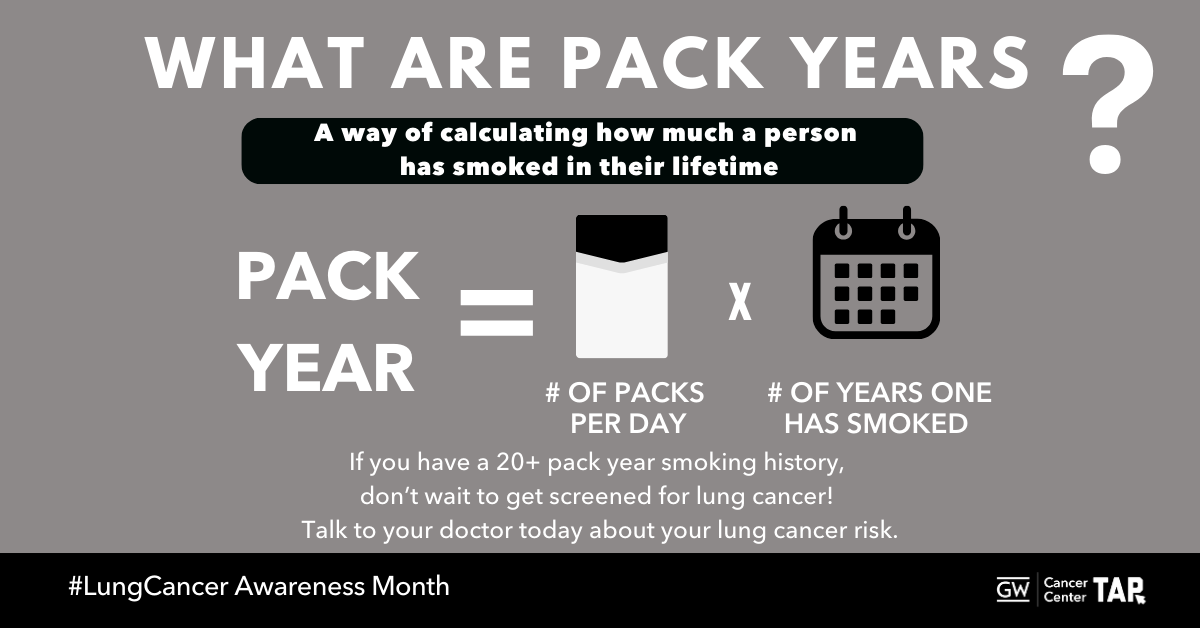 Download Image |
The @nationalcancerinstitute Cancer Information Service can answer your questions about lung cancer. Learn more at cancer.gov/contact #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Curious about radon? The CDC has information to find out how to protect your home and health today: http://bit.ly/2wxvd2u #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer is just the beginning. Follow-up care, support, and lifestyle changes can play an important role in your journey. Learn about survivorship resources available to you. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Caring for someone with cancer? The American Cancer Society’s Caregiver Resource Guide offers valuable tools and support. Access the guide here: https://bit.ly/4hu47QJ #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The National LGBTQ+ Cancer Network provides resources for cancer patients, clinicians, and caregivers. Find support tailored to your needs: https://bit.ly/2YgF0rO #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| ¿Vives en una zona con altos niveles de radón? Mira este video informativo sobre la exposición al radón y consejos para mitigarlo. Protege tu hogar y tu salud hoy: http://bit.ly/2wxvd2u #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Dar el primer paso hacia la prevención del cáncer de pulmón puede ser tan sencillo como una conversación con su médico. Si tiene más de 50 años y tiene antecedentes de tabaquismo, pregunte acerca de si la prueba de detección del cáncer de pulmón es adecuada para usted. #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The American College of Radiology can help you find a certified lung cancer screening center near you. Start your search here: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Lung cancer often has no symptoms until it’s advanced. Screening can find cancer early, when treatment is likely to work best. This November, ask about lung cancer screening if you’re 50 or older and smoked regularly in the past 15 years. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Delaying lung cancer screening because it may cost too much? There is help! Don’t assume you won’t qualify. Check your regional program today: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer involves more than treatment—it’s about ongoing care and support. Make a plan for long-term health and wellness. Explore these resources and make a plan for long-term health and wellness. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Looking for information about #lungcancer clinical trials? Check out these resources: https://bit.ly/3C8EqVM #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Everyone affected by #lungcancer needs a guide. Access resources to get you on the right track: https://bit.ly/3NOKzJy #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| If you currently or used to smoke, Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 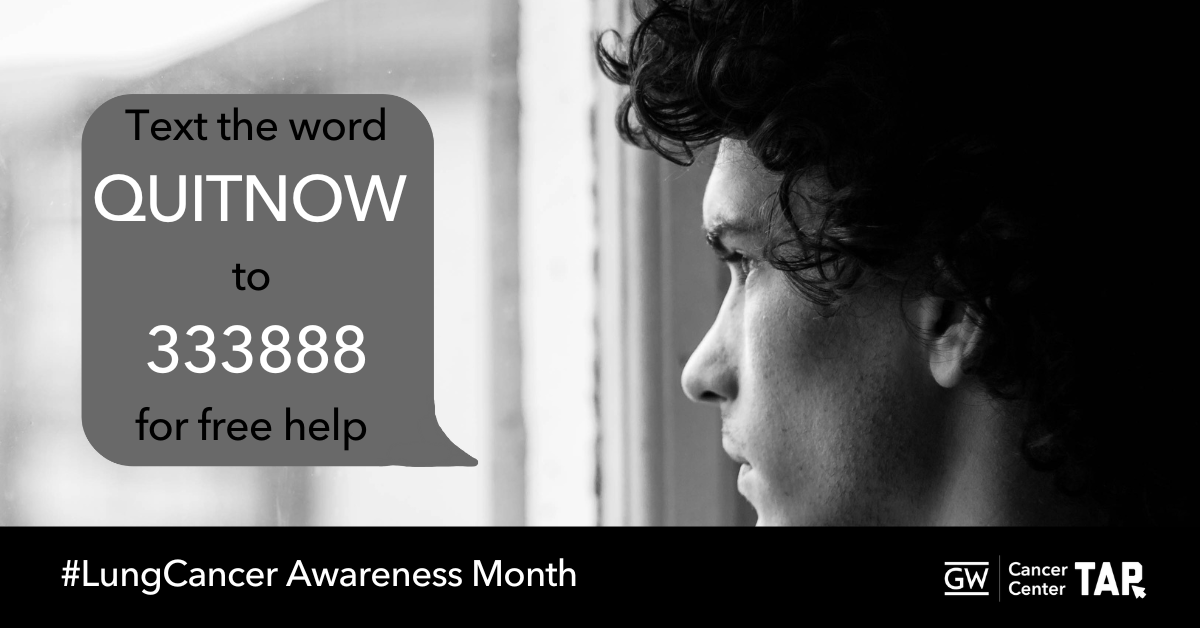 Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screening can detect cancer early, when it’s easier to treat. If you’re 50 or older and smoked regularly in the past 15 years, don’t wait—talk to your doctor about getting your annual screening today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Message | Suggested Graphic |
|---|---|
November is Lung Cancer Awareness Month. Early detection saves lives. If you’re over 50 and previously or currently smoke, lung cancer screening is recommended for some people who are at high risk! #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| It’s Lung Cancer Awareness Month. Screenings can catch cancer early when it’s more treatable. If you have smoked tobacco and are over 50-years-old, don’t wait. Ask your doctor about lung cancer screening. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screenings can find cancer early, when it’s easier to treat. If you smoke now or smoked tobacco regularly in the past and are at least 50 years old, don’t wait—talk to your doctor about getting screened today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 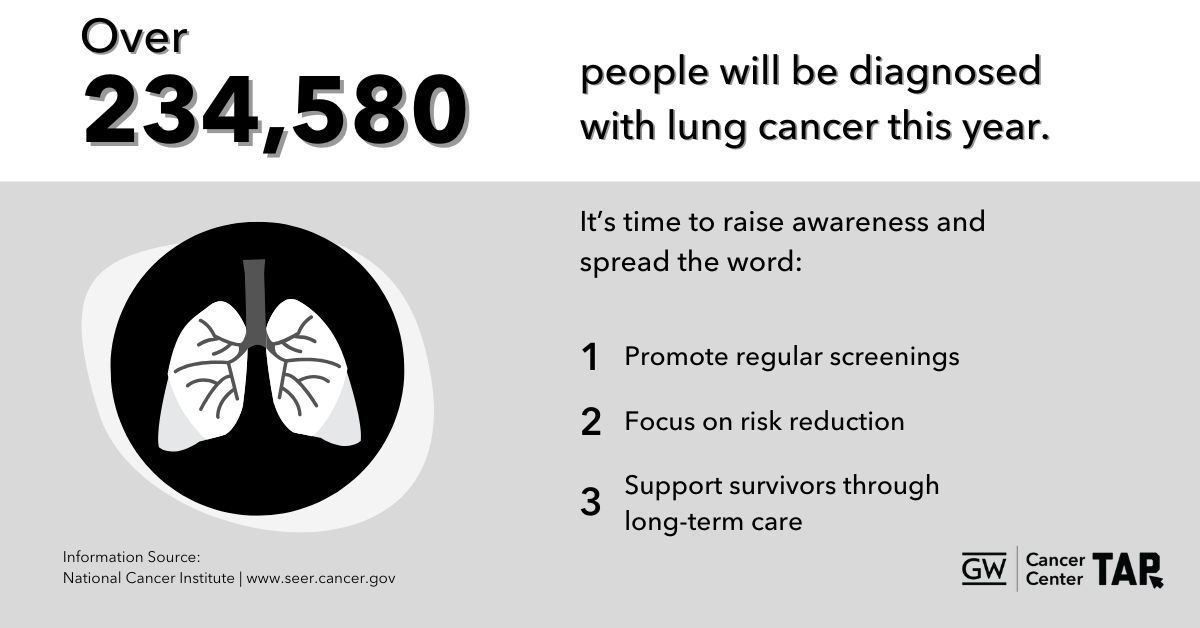 Download Image |
| [November 9th] It’s National Lung Cancer Screening Day! Screening can find lung cancer early, when it’s most treatable. If you are 50 years or older with a history of regular smoking—don’t wait. Get screened today and take control of your health. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| [November 9th] Lung cancer screenings are quick and can make a difference. If your doctor recommends lung screening, they do NOT think you have lung cancer, they’re just checking! Contact your doctor today to learn more. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Did you know? Lung cancer screenings can detect cancer early, when it’s easier to treat. If you are age 50+, don’t wait—talk to your doctor about whether screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 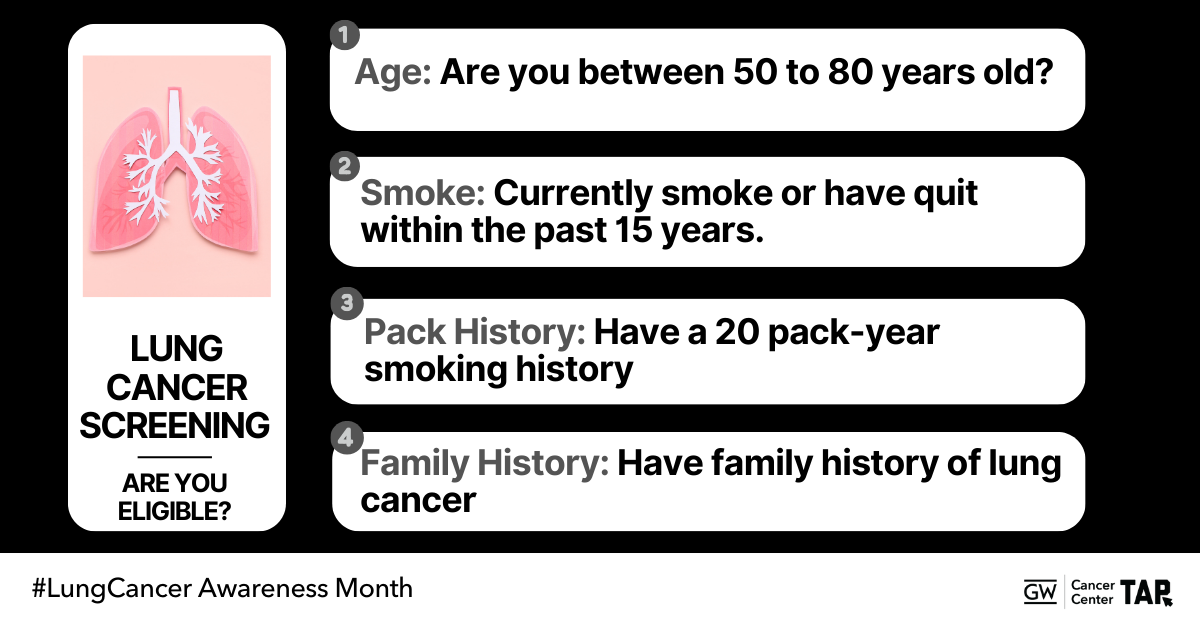 Download Image |
| Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives! #LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 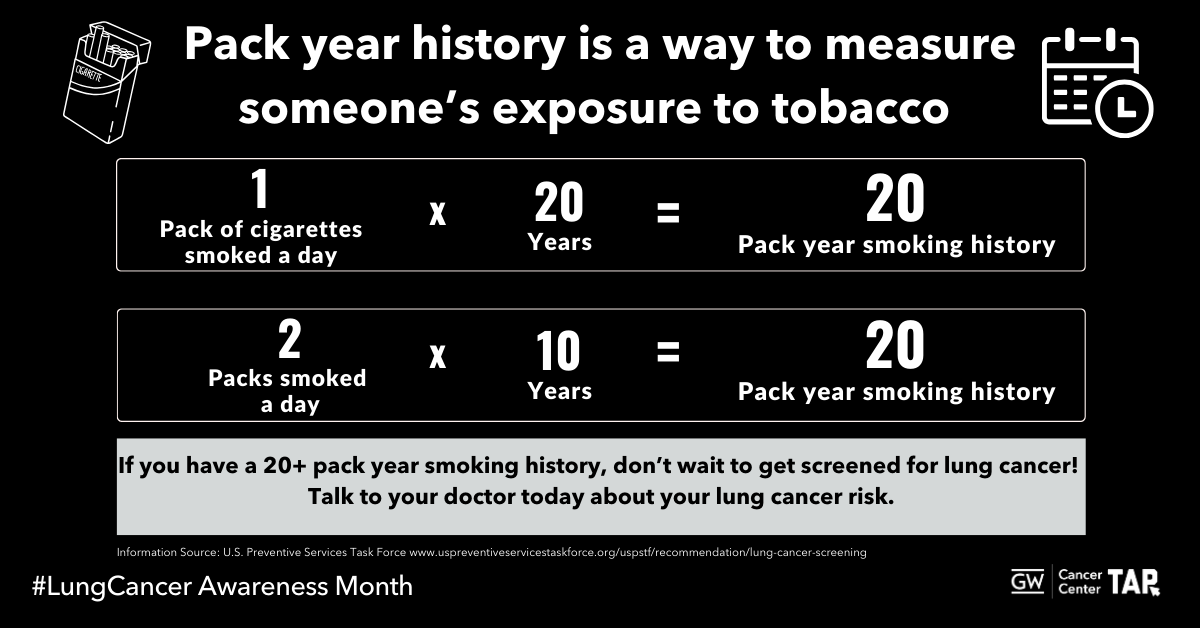 Download Image |
Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives!#LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 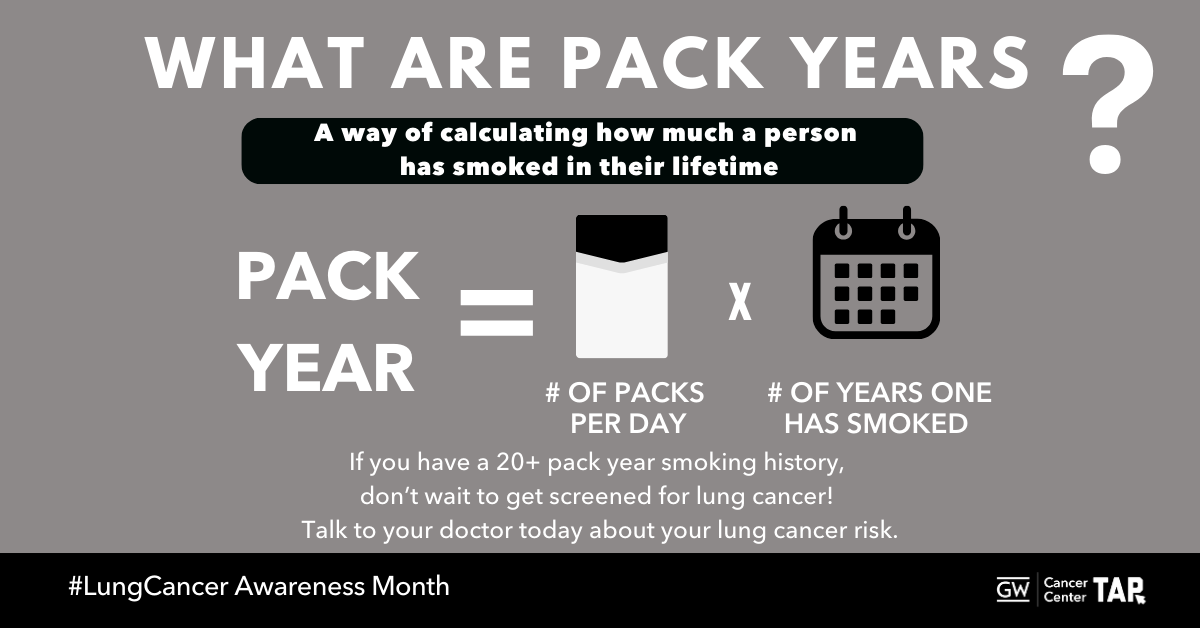 Download Image |
The @nationalcancerinstitute Cancer Information Service can answer your questions about lung cancer. Learn more at cancer.gov/contact #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Curious about radon? The CDC has information to find out how to protect your home and health today: http://bit.ly/2wxvd2u #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer is just the beginning. Follow-up care, support, and lifestyle changes can play an important role in your journey. Learn about survivorship resources available to you. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Caring for someone with cancer? The American Cancer Society’s Caregiver Resource Guide offers valuable tools and support. Access the guide here: https://bit.ly/4hu47QJ #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The National LGBTQ+ Cancer Network provides resources for cancer patients, clinicians, and caregivers. Find support tailored to your needs: https://bit.ly/2YgF0rO #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| ¿Vives en una zona con altos niveles de radón? Mira este video informativo sobre la exposición al radón y consejos para mitigarlo. Protege tu hogar y tu salud hoy: http://bit.ly/2wxvd2u #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Dar el primer paso hacia la prevención del cáncer de pulmón puede ser tan sencillo como una conversación con su médico. Si tiene más de 50 años y tiene antecedentes de tabaquismo, pregunte acerca de si la prueba de detección del cáncer de pulmón es adecuada para usted. #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The American College of Radiology can help you find a certified lung cancer screening center near you. Start your search here: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Lung cancer often has no symptoms until it’s advanced. Screening can find cancer early, when treatment is likely to work best. This November, ask about lung cancer screening if you’re 50 or older and smoked regularly in the past 15 years. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Delaying lung cancer screening because it may cost too much? There is help! Don’t assume you won’t qualify. Check your regional program today: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer involves more than treatment—it’s about ongoing care and support. Make a plan for long-term health and wellness. Explore these resources and make a plan for long-term health and wellness. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Looking for information about #lungcancer clinical trials? Check out these resources: https://bit.ly/3C8EqVM #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Everyone affected by #lungcancer needs a guide. Access resources to get you on the right track: https://bit.ly/3NOKzJy #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| If you currently or used to smoke, Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screening can detect cancer early, when it’s easier to treat. If you’re 50 or older and smoked regularly in the past 15 years, don’t wait—talk to your doctor about getting your annual screening today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Message | Suggested Graphic |
|---|---|
November is Lung Cancer Awareness Month. Early detection saves lives. If you’re over 50 and previously or currently smoke, lung cancer screening is recommended for some people who are at high risk! #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| It’s Lung Cancer Awareness Month. Screenings can catch cancer early when it’s more treatable. If you have smoked tobacco and are over 50-years-old, don’t wait. Ask your doctor about lung cancer screening. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screenings can find cancer early, when it’s easier to treat. If you smoke now or smoked tobacco regularly in the past and are at least 50 years old, don’t wait—talk to your doctor about getting screened today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 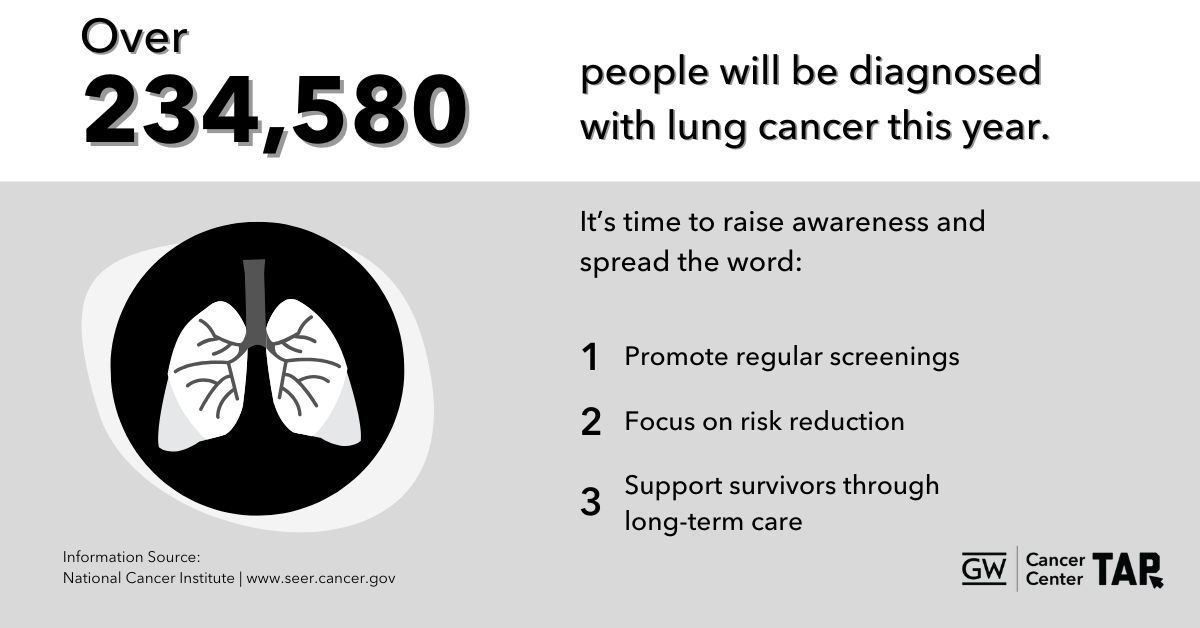 Download Image |
| [November 9th] It’s National Lung Cancer Screening Day! Screening can find lung cancer early, when it’s most treatable. If you are 50 years or older with a history of regular smoking—don’t wait. Get screened today and take control of your health. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| [November 9th] Lung cancer screenings are quick and can make a difference. If your doctor recommends lung screening, they do NOT think you have lung cancer, they’re just checking! Contact your doctor today to learn more. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Did you know? Lung cancer screenings can detect cancer early, when it’s easier to treat. If you are age 50+, don’t wait—talk to your doctor about whether screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 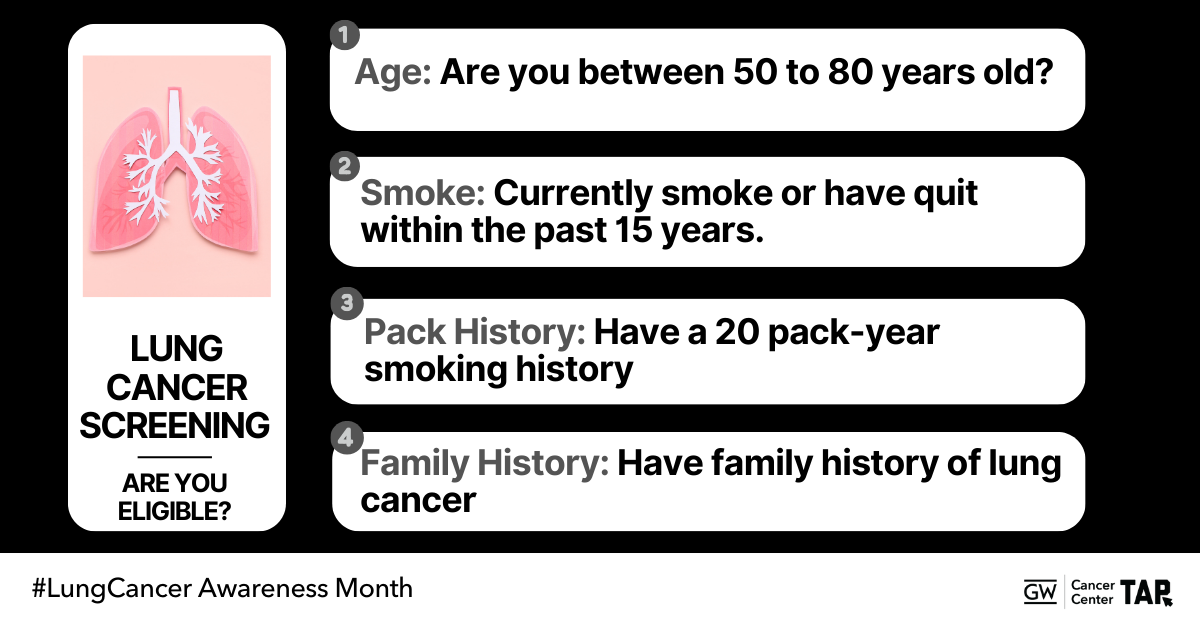 Download Image |
| Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives! #LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 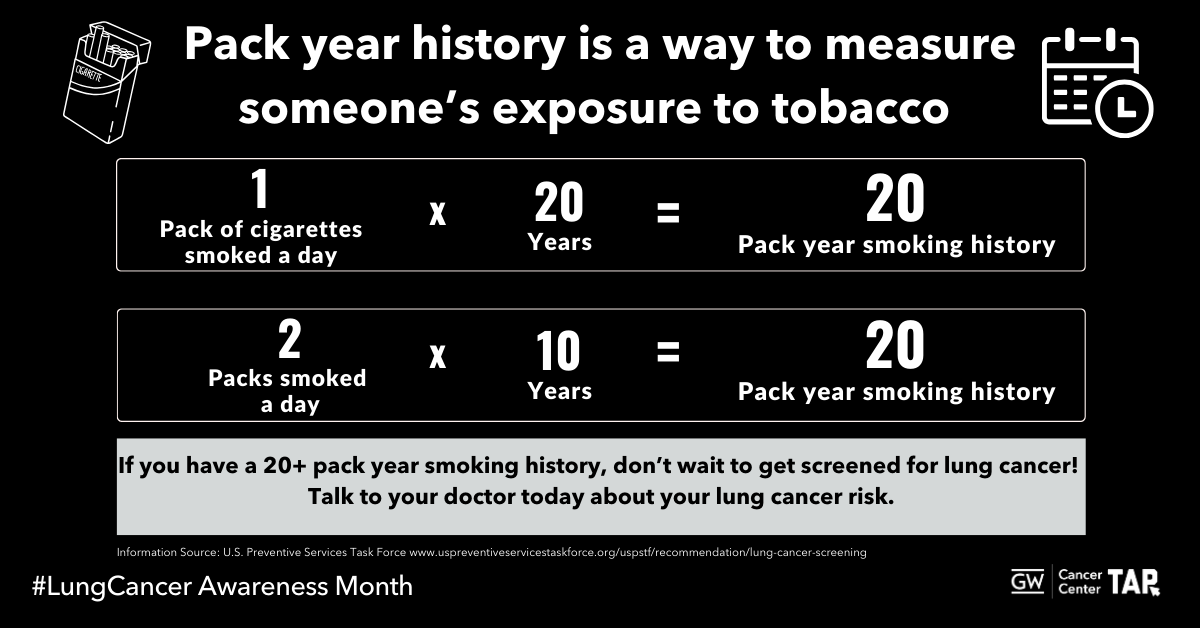 Download Image |
Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives!#LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 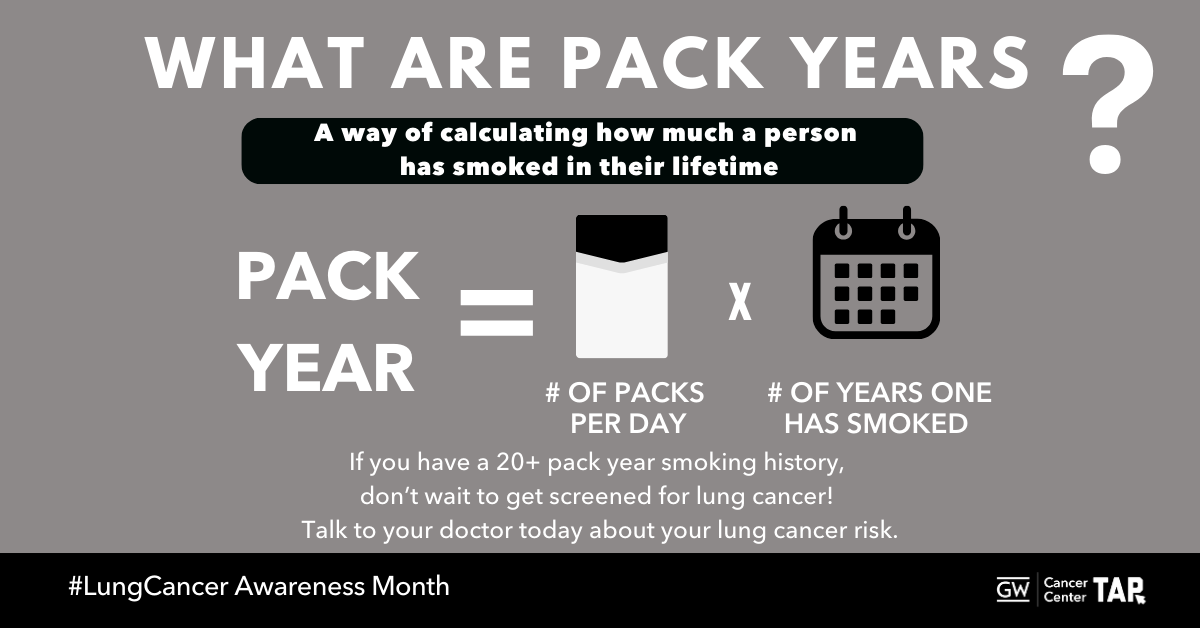 Download Image |
The @nationalcancerinstitute Cancer Information Service can answer your questions about lung cancer. Learn more at cancer.gov/contact #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 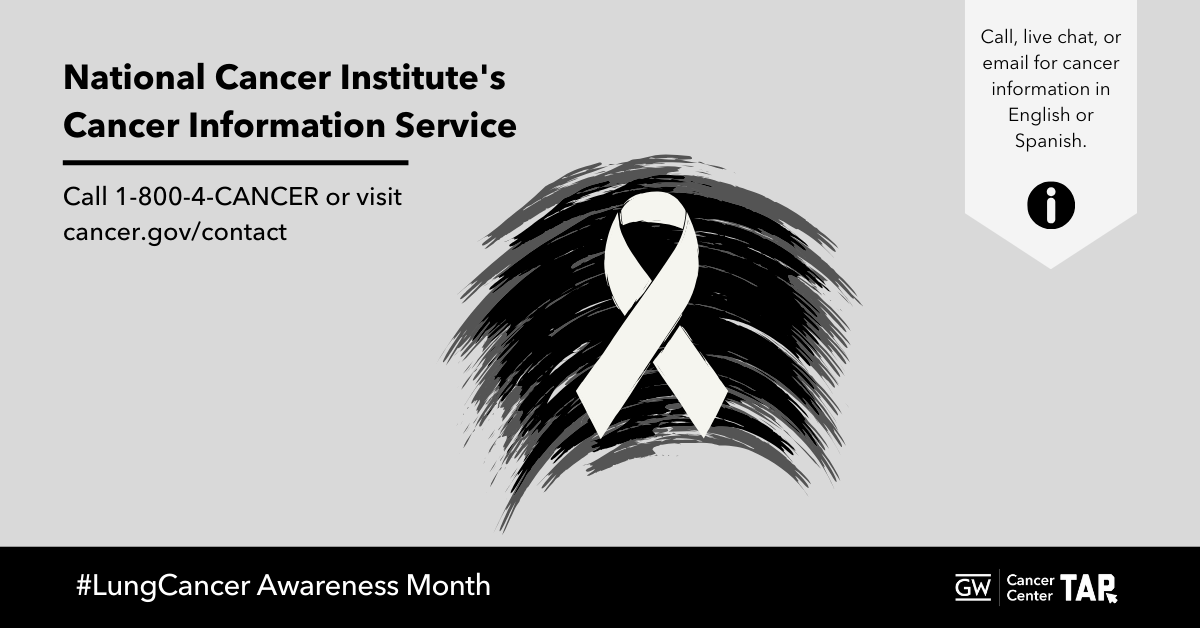 Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 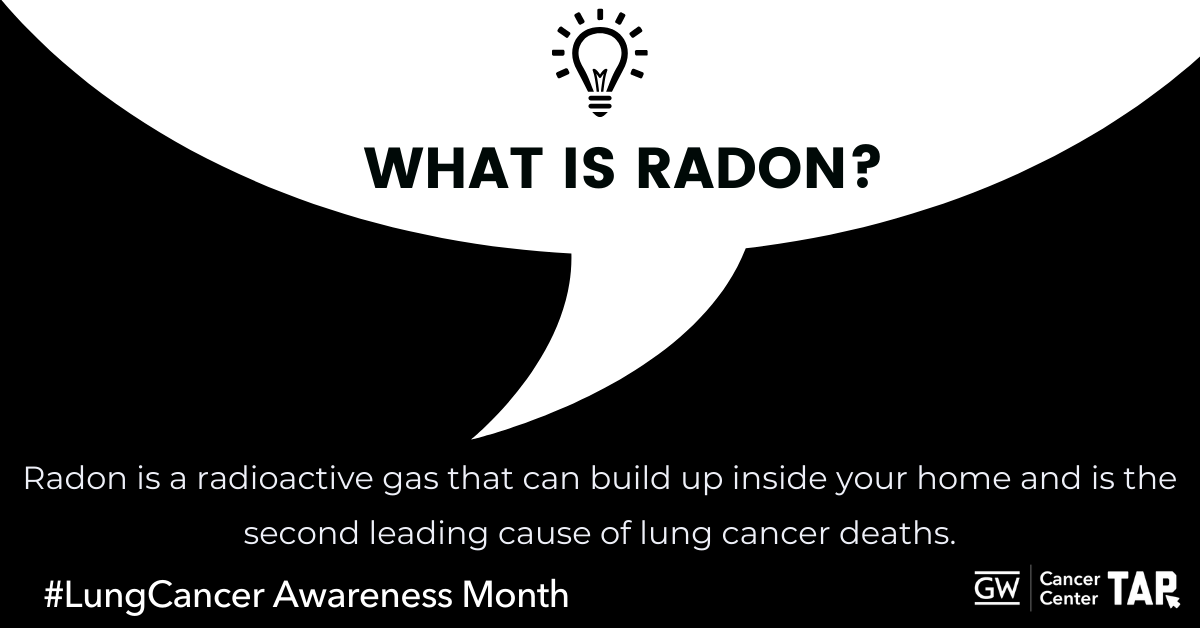 Download Image |
| Curious about radon? The CDC has information to find out how to protect your home and health today: http://bit.ly/2wxvd2u #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer is just the beginning. Follow-up care, support, and lifestyle changes can play an important role in your journey. Learn about survivorship resources available to you. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Caring for someone with cancer? The American Cancer Society’s Caregiver Resource Guide offers valuable tools and support. Access the guide here: https://bit.ly/4hu47QJ #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The National LGBTQ+ Cancer Network provides resources for cancer patients, clinicians, and caregivers. Find support tailored to your needs: https://bit.ly/2YgF0rO #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| ¿Vives en una zona con altos niveles de radón? Mira este video informativo sobre la exposición al radón y consejos para mitigarlo. Protege tu hogar y tu salud hoy: http://bit.ly/2wxvd2u #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Dar el primer paso hacia la prevención del cáncer de pulmón puede ser tan sencillo como una conversación con su médico. Si tiene más de 50 años y tiene antecedentes de tabaquismo, pregunte acerca de si la prueba de detección del cáncer de pulmón es adecuada para usted. #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The American College of Radiology can help you find a certified lung cancer screening center near you. Start your search here: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Lung cancer often has no symptoms until it’s advanced. Screening can find cancer early, when treatment is likely to work best. This November, ask about lung cancer screening if you’re 50 or older and smoked regularly in the past 15 years. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Delaying lung cancer screening because it may cost too much? There is help! Don’t assume you won’t qualify. Check your regional program today: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer involves more than treatment—it’s about ongoing care and support. Make a plan for long-term health and wellness. Explore these resources and make a plan for long-term health and wellness. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Looking for information about #lungcancer clinical trials? Check out these resources: https://bit.ly/3C8EqVM #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Everyone affected by #lungcancer needs a guide. Access resources to get you on the right track: https://bit.ly/3NOKzJy #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| If you currently or used to smoke, Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 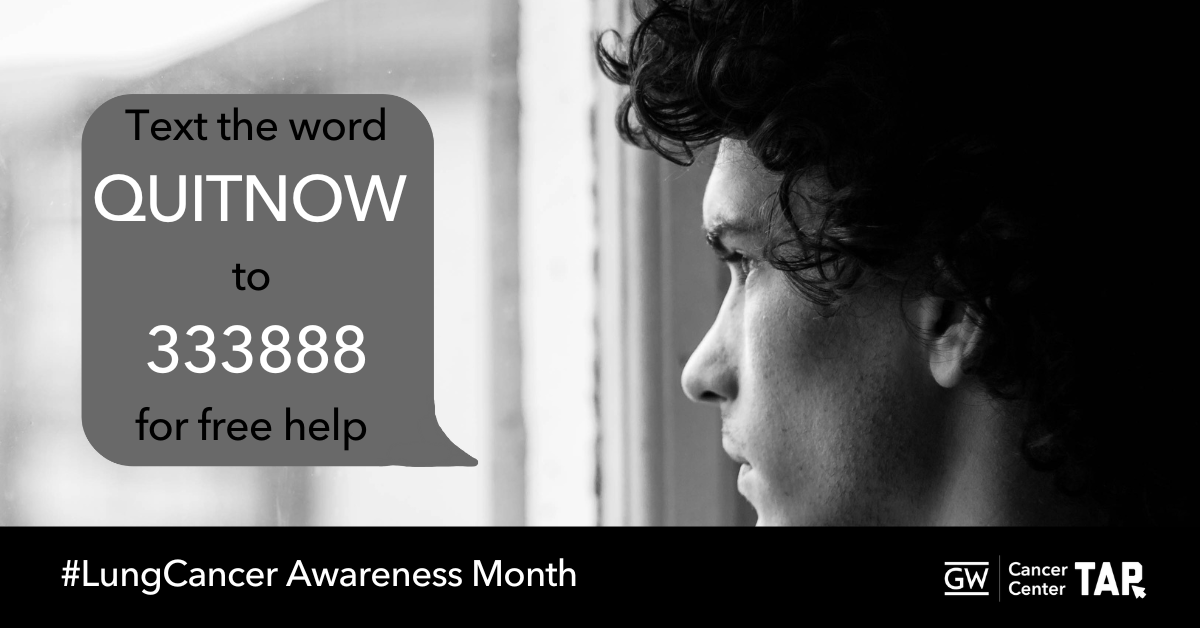 Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screening can detect cancer early, when it’s easier to treat. If you’re 50 or older and smoked regularly in the past 15 years, don’t wait—talk to your doctor about getting your annual screening today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Message | Suggested Graphic |
|---|---|
November is Lung Cancer Awareness Month. Early detection saves lives. If you’re over 50 and previously or currently smoke, lung cancer screening is recommended for some people who are at high risk! #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| It’s Lung Cancer Awareness Month. Screenings can catch cancer early when it’s more treatable. If you have smoked tobacco and are over 50-years-old, don’t wait. Ask your doctor about lung cancer screening. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screenings can find cancer early, when it’s easier to treat. If you smoke now or smoked tobacco regularly in the past and are at least 50 years old, don’t wait—talk to your doctor about getting screened today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 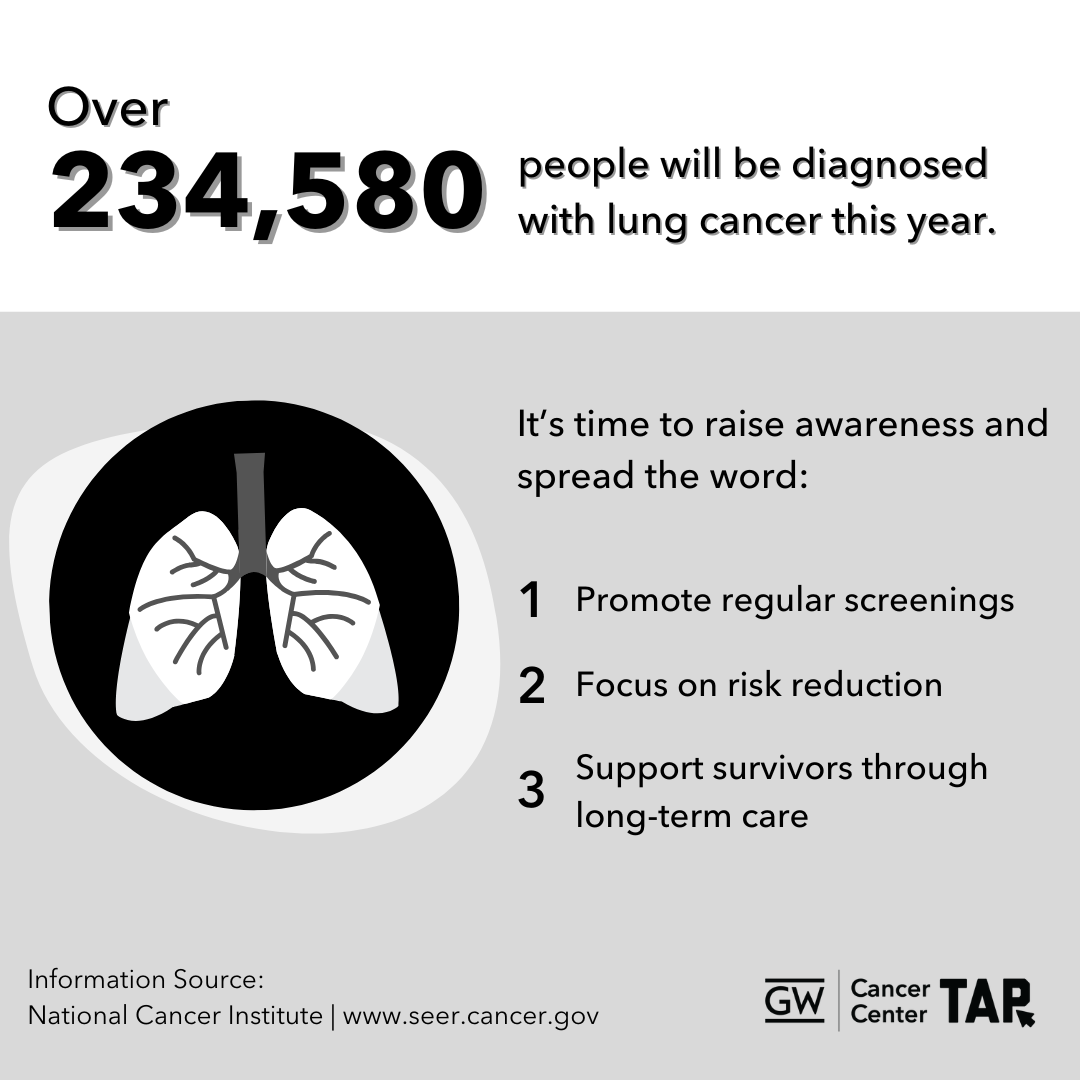 Download Image |
| [November 9th] It’s National Lung Cancer Screening Day! Screening can find lung cancer early, when it’s most treatable. If you are 50 years or older with a history of regular smoking—don’t wait. Get screened today and take control of your health. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| [November 9th] Lung cancer screenings are quick and can make a difference. If your doctor recommends lung screening, they do NOT think you have lung cancer, they’re just checking! Contact your doctor today to learn more. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Did you know? Lung cancer screenings can detect cancer early, when it’s easier to treat. If you are age 50+, don’t wait—talk to your doctor about whether screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 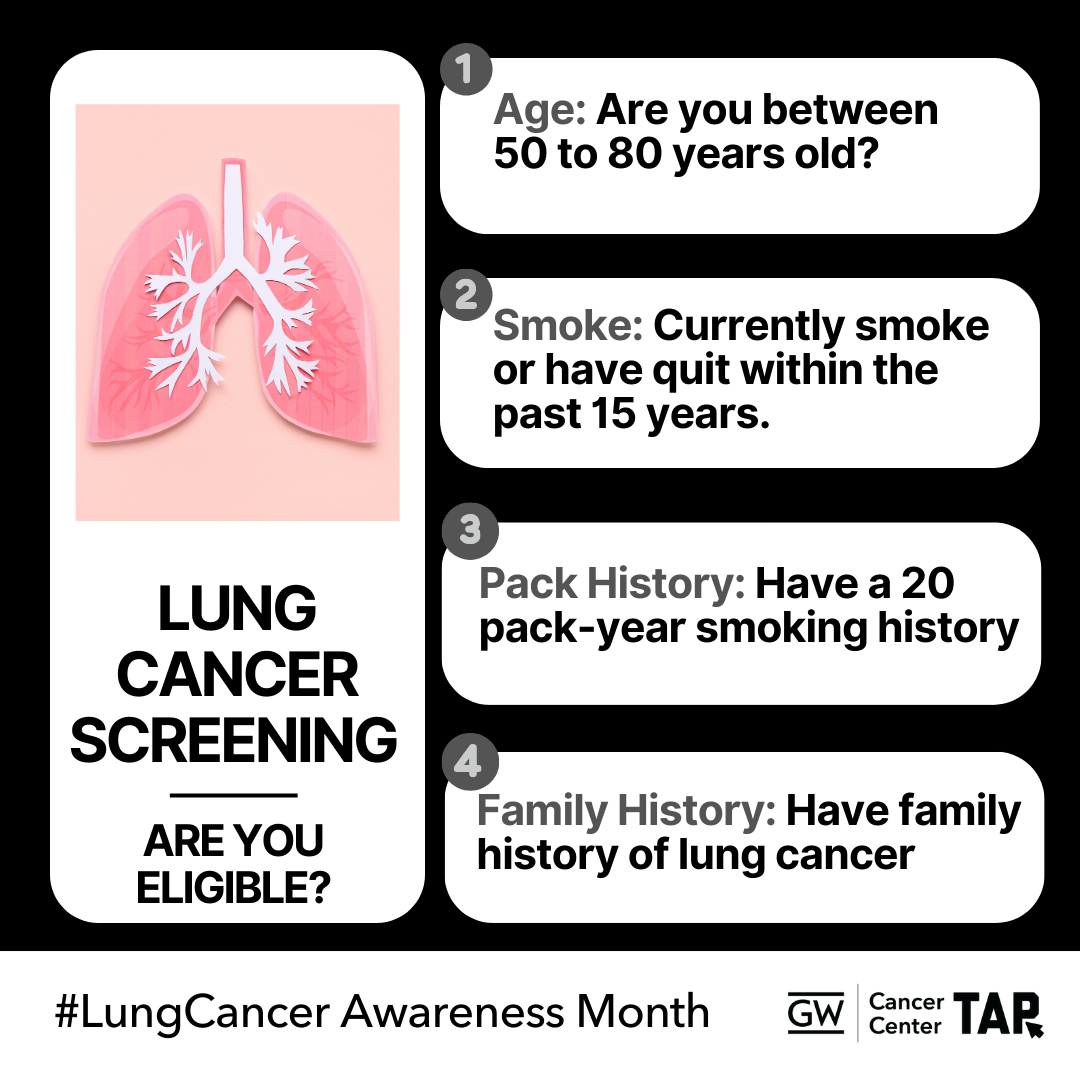 Download Image |
| Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives! #LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 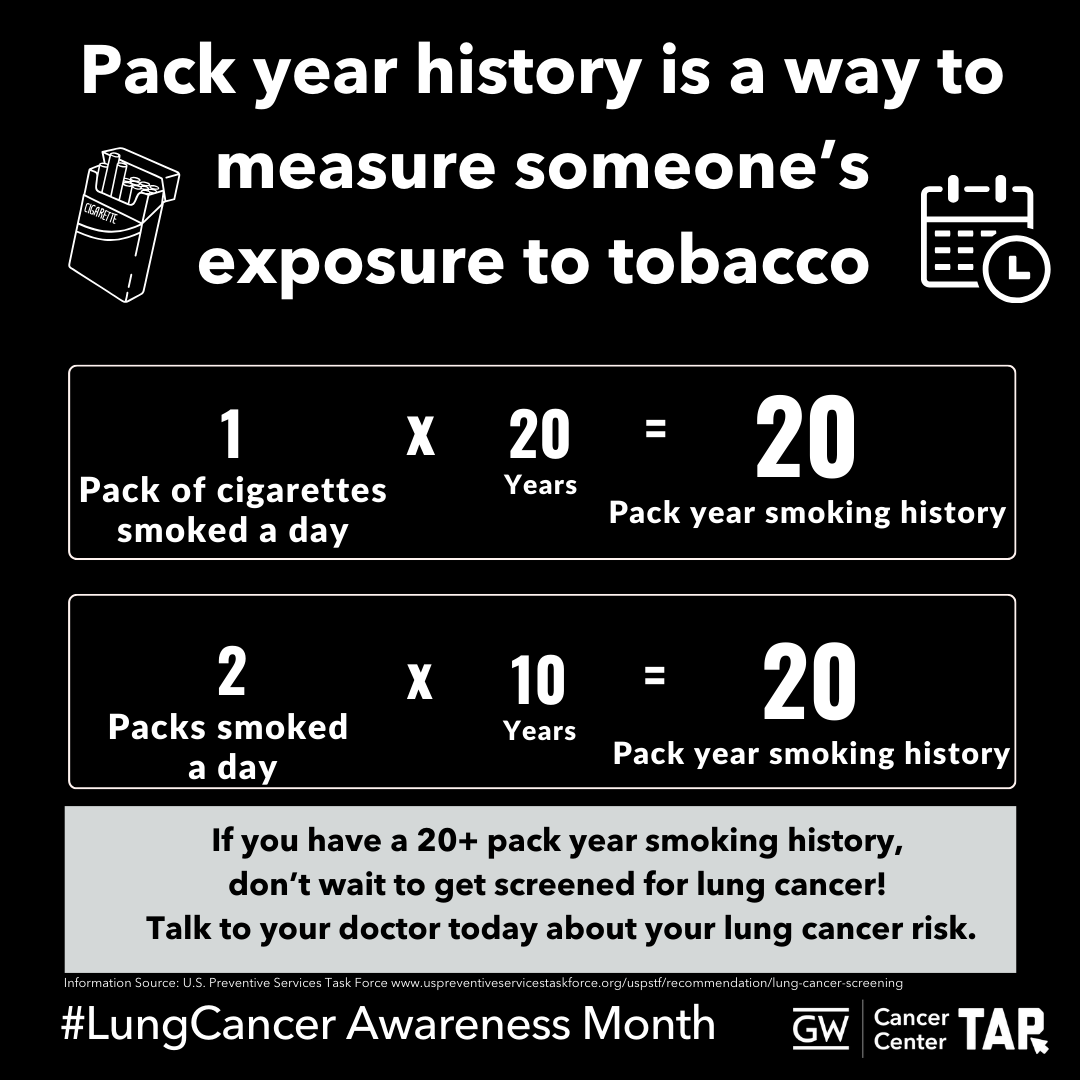 Download Image |
Did you know? Pack years are a way to measure lung cancer risk. Don’t wait to talk to your doctor about lung cancer screening, early detection saves lives! #LungCancerAwareness #GetScreened #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 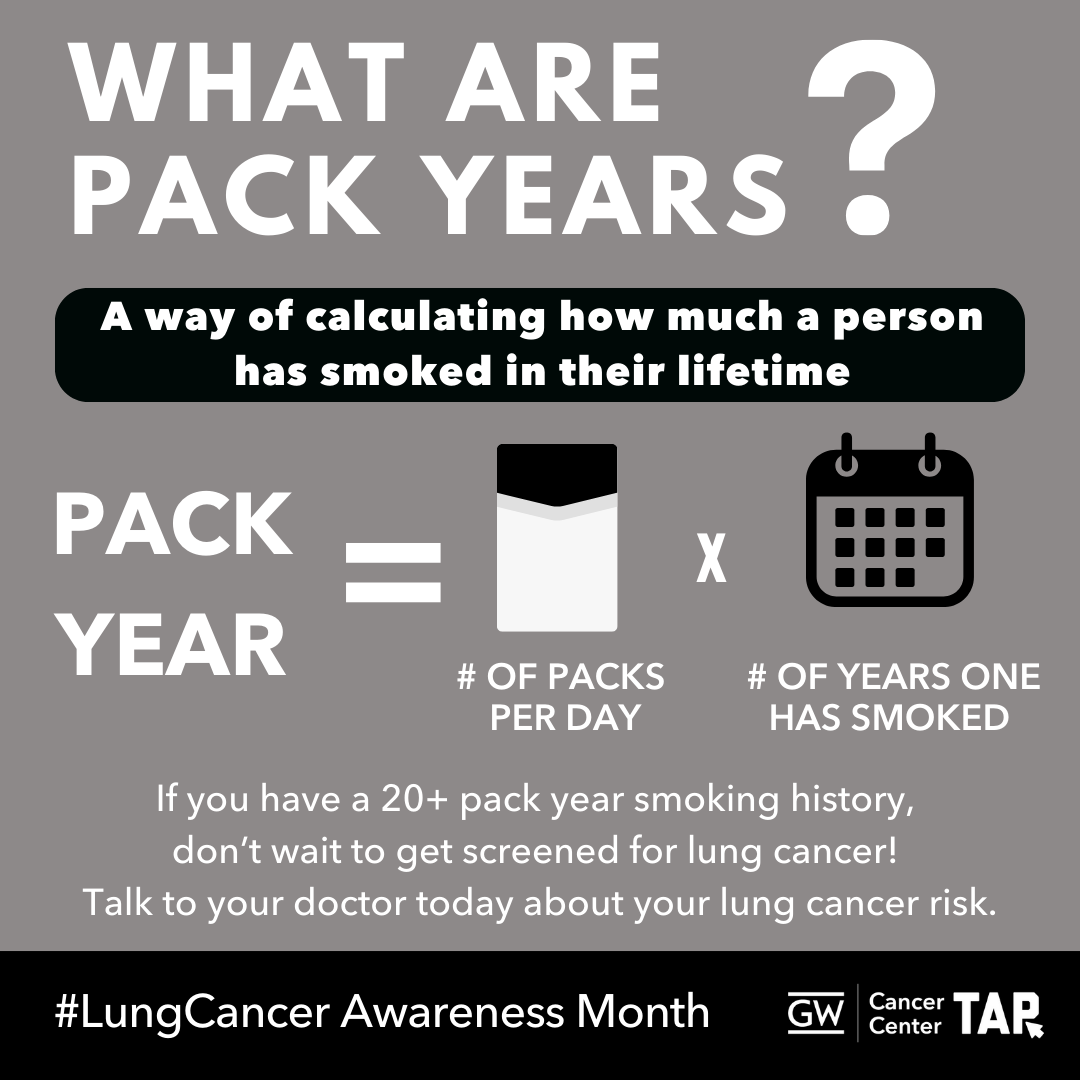 Download Image |
The @nationalcancerinstitute Cancer Information Service can answer your questions about lung cancer. Learn more at cancer.gov/contact #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 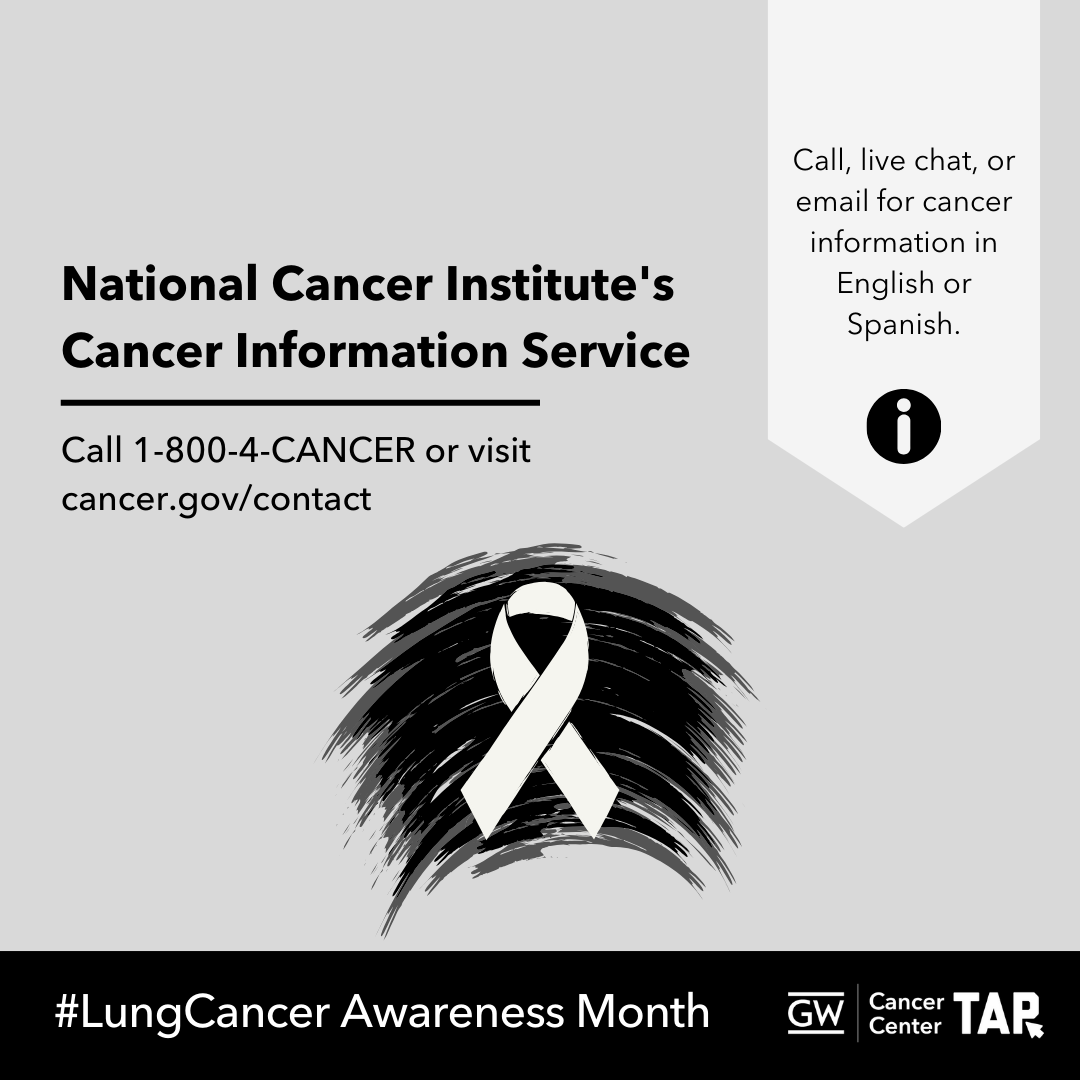 Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer | 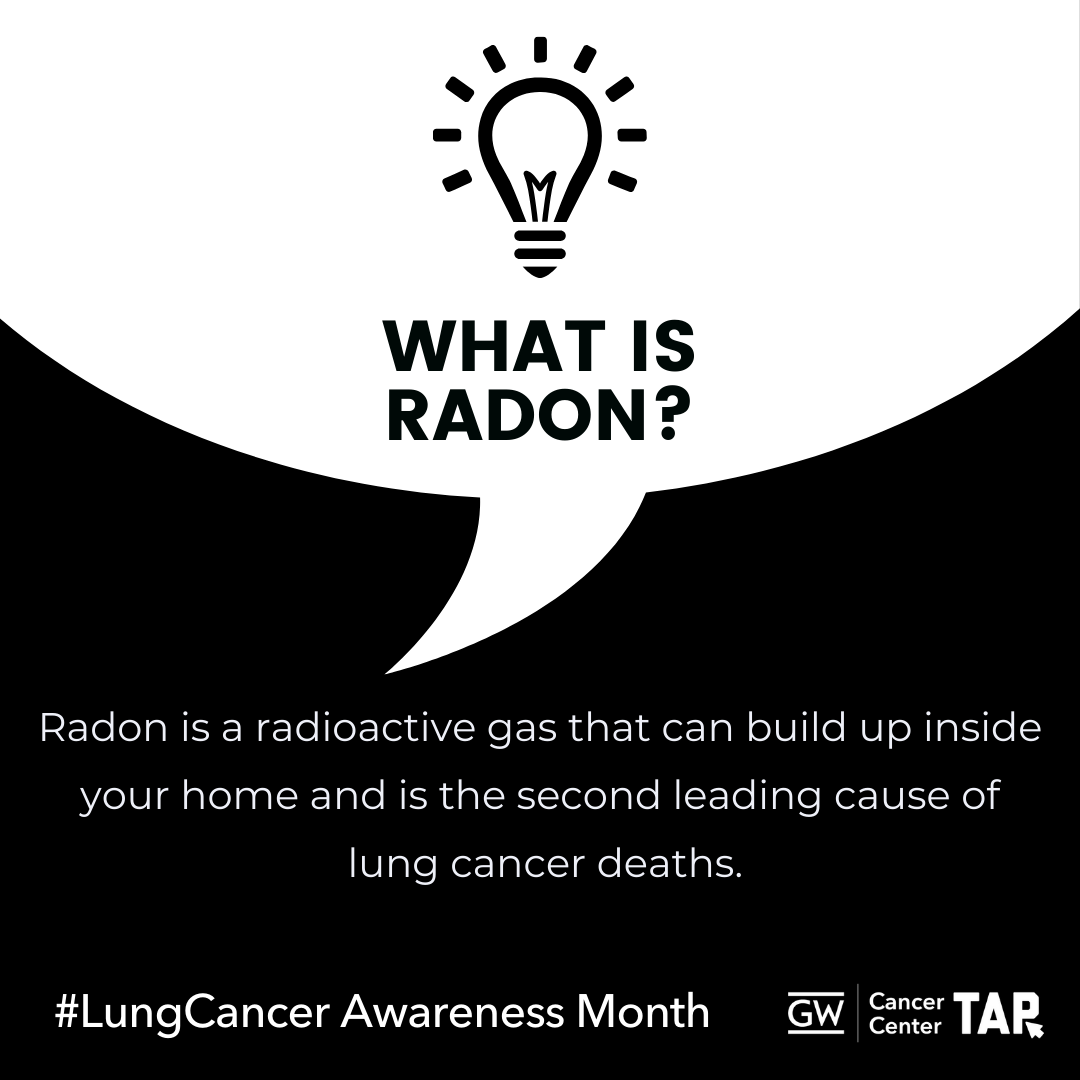 Download Image |
| Curious about radon? The CDC has information to find out how to protect your home and health today: http://bit.ly/2wxvd2u #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer is just the beginning. Follow-up care, support, and lifestyle changes can play an important role in your journey. Learn about survivorship resources available to you. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Caring for someone with cancer? The American Cancer Society’s Caregiver Resource Guide offers valuable tools and support. Access the guide here: https://bit.ly/4hu47QJ #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Taking the first step toward better health can be as simple as talking with your doctor. If you’re 50+ and have a history of smoking, ask if lung cancer screening is right for you. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The National LGBTQ+ Cancer Network provides resources for cancer patients, clinicians, and caregivers. Find support tailored to your needs: https://bit.ly/2YgF0rO #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Smoking isn’t the only thing that can cause lung cancer. Radon exposure also plays a role. Check your home for radon and discuss your risk with your doctor. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| ¿Vives en una zona con altos niveles de radón? Mira este video informativo sobre la exposición al radón y consejos para mitigarlo. Protege tu hogar y tu salud hoy: http://bit.ly/2wxvd2u #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Dar el primer paso hacia la prevención del cáncer de pulmón puede ser tan sencillo como una conversación con su médico. Si tiene más de 50 años y tiene antecedentes de tabaquismo, pregunte acerca de si la prueba de detección del cáncer de pulmón es adecuada para usted. #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| The American College of Radiology can help you find a certified lung cancer screening center near you. Start your search here: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Lung cancer often has no symptoms until it’s advanced. Screening can find cancer early, when treatment is likely to work best. This November, ask about lung cancer screening if you’re 50 or older and smoked regularly in the past 15 years. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Delaying lung cancer screening because it may cost too much? There is help! Don’t assume you won’t qualify. Check your regional program today: https://bit.ly/3YppHgN #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Surviving lung cancer involves more than treatment—it’s about ongoing care and support. Make a plan for long-term health and wellness. Explore these resources and make a plan for long-term health and wellness. https://bit.ly/3YIPFx3 #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Looking for information about #lungcancer clinical trials? Check out these resources: https://bit.ly/3C8EqVM #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Everyone affected by #lungcancer needs a guide. Access resources to get you on the right track: https://bit.ly/3NOKzJy #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| If you currently or used to smoke, Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Ready to quit smoking? The CDC provides free resources to help you stop smoking and improve your health. Call 1-800-QUIT-NOW or text QUITNOW to 333888 for support: https://bit.ly/3A94wri #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
| Did you know? Lung cancer screening can detect cancer early, when it’s easier to treat. If you’re 50 or older and smoked regularly in the past 15 years, don’t wait—talk to your doctor about getting your annual screening today. #LungCancerAwareness #GetScreened #EarlyDetection #GWCCTAP #TAPintoCancerControl #TAPforLungCancer |  Download Image |
Download All Messages and Graphics
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets below can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Download All LinkedIn, Facebook or Twitter Messages
Download All Instagram Messages
If you would like to download all images in this social media toolkit, click on each network below for a zip file with each network’s graphics. Please note that these image sizes are slightly smaller than the links above due to file size limitations. If you would like to download full resolution versions, simply click on the “Download Graphic” link below each image in the message tables above.
Download all LinkedIn, Facebook or Twitter Graphics
Download All Instagram Graphics
Template Graphics
Want to add your logo or customize these graphics? Use these helpful Canva links to access our templates.
Footnotes
1. Centers for Disease Control and Prevention (2024). Lung Cancer Statistics. Retrieved from https://www.cdc.gov/lung-cancer/statistics/index.html
2. U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention. (2024). Cancer statistics data visualization tool, based on 2021 submission data. Retrieved from https://gis.cdc.gov/Cancer/USCS/#/AtAGlance
3.U.S. Cancer Statistics Working Group, 2024.
4. U.S. Cancer Statistics Working Group, 2024.
5. Centers for Disease Control and Prevention (2024). State Cancer Profiles. Retrieved from https://statecancerprofiles.cancer.gov/index.html
6. Philipson, T. J., Durie, T., Cong, Z., & Fendrick, A. M. (2023). The aggregate value of cancer screenings in the United States: full potential value and value considering adherence. BMC health services research, 23(1), 829. https://doi.org/10.1186/s12913-023-09738-4″
7. American Lung Association. (2024). Lung Cancer Key Findings. https://www.lung.org/research/state-of-lung-cancer/key-findings
8. Centers for Disease Control and Prevention (2023). Lung Cancer Risk Factors. Retrieved from https://www.cdc.gov/lung-cancer/risk-factors/index.html
9. Alduais, Y., Zhang, H., Fan, F., Chen, J., & Chen, B. (2023). Non-small cell lung cancer (NSCLC): A review of risk factors, diagnosis, and treatment. Medicine, 102(8), e32899. https://doi.org/10.1097/MD.0000000000032899
10. Turner, J., Pond, G. R., Tremblay, A., Johnston, M., Goss, G., Nicholas, G., Martel, S., Bhatia, R., Liu, G., Schmidt, H., Tammemagi, M. C., Puksa, S., Atkar-Khattra, S., Tsao, M. S., Lam, S., & Goffin, J. R. (2021). Risk Perception Among a Lung Cancer Screening Population. Chest, 160(2), 718–730. https://doi.org/10.1016/j.chest.2021.02.050
11. Riudavets, M., Garcia de Herreros, M., Besse, B., & Mezquita, L. (2022). Radon and Lung Cancer: Current Trends and Future Perspectives. Cancers, 14(13), 3142. https://doi.org/10.3390/cancers14133142
12. Centers for Disease Control and Prevention (2023). Lung Cancer Among People Who Never Smoked. Retrieved from https://www.cdc.gov/lung-cancer/nonsmokers/index.html
13. U.S. Preventive Services Task Force (2021). Lung Cancer: Screening. Retrieved from https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
14. Carter-Bawa, L., Banerjee, S. C., Comer, R. S., Kale, M. S., King, J. C., Leopold, K. T., Monahan, P. O., Ostroff, J. S., Slaven, J. E., Jr, Valenzona, F., Wiener, R. S., & Rawl, S. M. (2023). Leveraging social media to increase lung cancer screening awareness, knowledge and uptake among high-risk populations (The INSPIRE-Lung Study): study protocol of design and methods of a community-based randomized controlled trial. BMC public health, 23(1), 975. https://doi.org/10.1186/s12889-023-15857-8 ; President’s Cancer Panel. (2022). Closing Gaps in Cancer Screening: Connecting People, Communities, and Systems to Improve Equity and Access. A Report from the President s Cancer Panel to the President of the United States. Retrieved from https://prescancerpanel.cancer.gov/report/cancerscreening/Part2Goal1.html
15. Lopez-Olivo, M. A., Maki, K. G., Choi, N. J., Hoffman, R. M., Shih, Y. T., Lowenstein, L. M., Hicklen, R. S., & Volk, R. J. (2020). Patient adherence to screening for lung cancer in the US: A systematic review and meta-analysis. JAMA Network Open, 3(11), e2025102. https://doi.org/10.1001/jamanetworkopen.2020.25102 ; Lin, Y., Liang, L., Ding, R., Prosper, A. E., Aberle, D. R., & Hsu, W. (2023). Factors associated with nonadherence to lung cancer screening across multiple screening time points. JAMA Network Open, 6(5), e2315250. https://doi.org/10.1001/jamanetworkopen.2023.15250
16. Arem, H., Mama, S. K., Duan, X., Rowland, J. H., Bellizzi, K. M., & Ehlers, D. K. (2020). Prevalence of healthy behaviors among cancer survivors in the United States: How far have we come? Cancer Epidemiology, Biomarkers & Prevention, 29(6), 1179–1187. https://doi.org/10.1158/1055-9965.EPI-19-1318 ; Back A. L. (2020). Patient-Clinician Communication Issues in Palliative Care for Patients With Advanced Cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 38(9), 866–876. https://doi.org/10.1200/JCO.19.00128
17. Back, 2020.
18. Sullivan, D. R., Chan, B., Lapidus, J. A., Ganzini, L., Hansen, L., Carney, P. A., Fromme, E. K., Marino, M., Golden, S. E., Vranas, K. C., & Slatore, C. G. (2019). Association of Early Palliative Care Use With Survival and Place of Death Among Patients With Advanced Lung Cancer Receiving Care in the Veterans Health Administration. JAMA oncology, 5(12), 1702–1709. https://doi.org/10.1001/jamaoncol.2019.3105
19. Serçekuş, P., Gencer, H., & Özkan, S. (2020). Finding useful cancer information may reduce cancer information overload for Internet users. Health information and libraries journal, 37(4), 319–328. https://doi.org/10.1111/hir.12325
20. Duncan, F. C., & Sears, C. R. (2020). Patient Perspectives on Shared Decision-Making in Lung Cancer Screening: To Teach or To Trust?. Chest, 158(3), 860–861. https://doi.org/10.1016/j.chest.2020.03.058 ; Golden, S. E., Ono, S. S., Thakurta, S. G., Wiener, R. S., Iaccarino, J. M., Melzer, A. C., Datta, S. K., & Slatore, C. G. (2020). “I’m Putting My Trust in Their Hands”: A Qualitative Study of Patients’ Views on Clinician Initial Communication About Lung Cancer Screening. Chest, 158(3), 1260–1267. https://doi.org/10.1016/j.chest.2020.02.072
21. Mitchell, J. A., Williams, E.-D. G., Li, Y., & Tarraf, W. (2020). Identifying disparities in patient-centered care experiences between non-Latino white and black men: Results from the 2008-2016 Medical Expenditure Panel Survey. BMC Health Services Research, 20(1), 495–495. https://doi.org/10.1186/s12913-020-05357-5
22. Rose, S., Boyes, A., Kelly, B., Cox, M., Palazzi, K., & Paul, C. (2021). Lung cancer stigma is a predictor for psychological distress: A longitudinal study. Lung cancer stigma is a predictor for psychological distress. Psycho-oncology, 30(7), 1137–1144. https://doi.org/10.1002/pon.5665 ; Rankin, N. M., McWilliams, A., & Marshall, H. M. (2020). Lung cancer screening implementation: Complexities and priorities. Respirology (Carlton, Vic.), 25 Suppl 2, 5–23. https://doi.org/10.1111/resp.13963
23. Banerjee, S. C., Haque, N., Schofield, E. A., Williamson, T. J., Martin, C. M., Bylund, C. L., Shen, M. J., Rigney, M., Hamann, H. A., Parker, P. A., McFarland, D. C., Park, B. J., Molena, D., Moreno, A., & Ostroff, J. S. (2021). Oncology Care f Training in Empathic Communication Skills to Reduce Lung Cancer Stigma. Chest, 159(5), 2040–2049. https://doi.org/10.1016/j.chest.2020.11.024 ; Carter-Bawa, L., Ostroff, J. S., Hoover, K., & Studts, J. L. (2023). Effective Communication About Lung Cancer Screening Without Iatrogenic Stigma: A Brief Report Case Study Using the Lung Cancer Stigma Communications Assessment Tool of LungTalk. JTO clinical and research reports, 4(11), 100585. https://doi.org/10.1016/j.jtocrr.2023.100585
24. Paige, S. R., Salloum, R. G., Krieger, J. L., Williams, M., Xue, W., & Brumback, B. (2020). Promoting clinical conversations about lung cancer screening: Exploring the role of perceived online social support. Journal of Health Communication, 25(8), 650–659. https://doi.org/10.1080/10810730.2020.1836087
25. Boatman, D., McCauley-Hixenbaugh, L., Starkey, A., Allen, A., & Kennedy-Rea, S. (2024). A new communication approach to encourage lung cancer screening action in rural eligible populations. PEC innovation, 4, 100298. https://doi.org/10.1016/j.pecinn.2024.100298
26. Williamson, T. J., Rawl, S. M., Kale, M. S., & Carter-Harris, L. (2021). Lung cancer screening and stigma: Do smoking-related differences in perceived lung cancer stigma emerge prior to diagnosis? Stigma and Health. https://doi.org/10.1037/sah0000300.supp
27. International Association for the Study of Lung Cancer (2021). IASLC Language Guide. Retrieved from https://www.iaslc.org/IASLCLanguageGuide
28. Hoffman, R. M., Reuland, D. S., & Volk, R. J. (2021). The Centers for Medicare & Medicaid Services Requirement for Shared Decision-making for Lung Cancer Screening. JAMA, 325(10), 933–934. https://doi.org/10.1001/jama.2021.1817
29. Choi, E., Ding, V. Y., Luo, S. J., & et al. (2023). Risk model–based lung cancer screening and racial and ethnic disparities in the US. JAMA Oncology, 9(12), 1640–1648. https://doi.org/10.1001/jamaoncol.2023.4447
30. Rivera, M. P., Katki, H. A., Tanner, N. T., Triplette, M., Sakoda, L. C., Wiener, R. S., Cardarelli, R., Carter-Harris, L., Crothers, K., Fathi, J. T., Ford, M. E., Smith, R., Winn, R. A., Wisnivesky, J. P., Henderson, L. M., & Aldrich, M. C. (2020). Addressing Disparities in Lung Cancer Screening Eligibility and Healthcare Access. An Official American Thoracic Society Statement. American journal of respiratory and critical care medicine, 202(7), e95–e112. https://doi.org/10.1164/rccm.202008-3053ST
31. Huo, J., Hong, Y. R., Bian, J., Guo, Y., Wilkie, D. J., & Mainous, A. G., 3rd (2019). Low Rates of Patient-Reported Physician-Patient Discussion about Lung Cancer Screening among Current Smokers: Data from Health Information National Trends Survey. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 28(5), 963–973. https://doi.org/10.1158/1055-9965.EPI-18-0629
32. Sakoda, L. C., Rivera, M. P., Zhang, J., & et al. (2021). Patterns and factors associated with adherence to lung cancer screening in diverse practice settings. JAMA Network Open, 4(4), e218559. https://doi.org/10.1001/jamanetworkopen.2021.8559
33. National Cancer Institute. (2020). Cancer disparities. https://www.cancer.gov/about-cancer/understanding/disparities
34. Giaquinto, A. N., Miller, K. D., Tossas, K. Y., Winn, R. A., Jemal, A., & Siegel, R. L. (2022). Cancer statistics for African American/Black People 2022. CA: a cancer journal for clinicians, 72(3), 202–229. https://doi.org/10.3322/caac.21718
35. Giaquinto et al. 2022.
36. Evans, N., 3rd, Grenda, T., Alvarez, N. H., & Okusanya, O. T. (2021). Narrative review of socioeconomic and racial disparities in the treatment of early stage lung cancer. Journal of thoracic disease, 13(6), 3758–3763. https://doi.org/10.21037/jtd-20-3181
37. American Lung Association (2020). State of Lung Cancer 2020: Racial and Ethnic Disparities. Retrieved from https://www.lung.org/research/state-of-lung-cancer/racial-and-ethnic-disparities
38. Evans et al. 2021.
39. Lake, M., Shusted, C. S., Juon, H. S., McIntire, R. K., Zeigler-Johnson, C., Evans, N. R., Kane, G. C., & Barta, J. A. (2020). Black patients referred to a lung cancer screening program experience lower rates of screening and longer time to follow-up. BMC cancer, 20(1), 561. https://doi.org/10.1186/s12885-020-06923-0
40. Lake et al. 2020.
41. Miller, K. D., Ortiz, A. P., Pinheiro, P. S., Bandi, P., Minihan, A., Fuchs, H. E., Martinez Tyson, D., Tortolero-Luna, G., Fedewa, S. A., Jemal, A. M., & Siegel, R. L. (2021). Cancer statistics for the US Hispanic/Latino population, 2021. CA: A Cancer Journal for Clinicians. https://doi.org/10.3322/caac.21695
42. American Lung Association (2020). State of Lung Cancer 2020: Racial and Ethnic Disparities. Retrieved from https://www.lung.org/research/state-of-lung-cancer/racial-and-ethnic-disparities
43. Cohen, R. A., & Cha, A. E. (2023). Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2022. National Center for Health Statistics. https://dx.doi.org/10.15620/cdc:127055 ; Olazagasti, C., & Seetharamu, N. (2021). Disparities in lung cancer screening rates among the Hispanic/LatinX population. Lung cancer management, 10(3), LMT51. https://doi.org/10.2217/lmt-2021-0004
44. Olazagasti and Seetharamu, 2021.
45. Lee, R. J., Madan, R. A., Kim, J., Posadas, E. M., & Yu, E. Y. (2021). Disparities in Cancer Care and the Asian American Population. The oncologist, 26(6), 453–460. https://doi.org/10.1002/onco.13748
46. Lee et al. 2021.
47. Lee et al. 2021.
48. American Lung Association (2020). State of Lung Cancer 2020: Racial and Ethnic Disparities. Retrieved from https://www.lung.org/research/state-of-lung-cancer/racial-and-ethnic-disparities
49. DeRouen, M. C., Canchola, A. J., Thompson, C. A., Jin, A., Nie, S., Wong, C., Lichtensztajn, D., Allen, L., Patel, M. I., Daida, Y. G., Luft, H. S., Shariff-Marco, S., Reynolds, P., Wakelee, H. A., Liang, S. Y., Waitzfelder, B. E., Cheng, I., & Gomez, S. L. (2022). Incidence of Lung Cancer Among Never-Smoking Asian American, Native Hawaiian, and Pacific Islander Females. Journal of the National Cancer Institute, 114(1), 78–86. https://doi.org/10.1093/jnci/djab143
50. Lee et al. 2021.
51. Lee et al. 2021.
52. Yom, S., & Lor, M. (2022). Advancing Health Disparities Research: The Need to Include Asian American Subgroup Populations. Journal of racial and ethnic health disparities, 9(6), 2248–2282. https://doi.org/10.1007/s40615-021-01164-8
53. Wills, T.A., Kaholokula, J.K., Pokhrel, P., Cassel, K. (2024). Risk and Protection for Lung Cancer Among Native Hawaiians and Pacific Islanders. In: Garvey, G. (eds) Indigenous and Tribal Peoples and Cancer. Springer, Cham. https://doi.org/10.1007/978-3-031-56806-0_40
54. Wills et al. 2024.
55. Wills et al. 2024.
56. DeRouen et al. 2022.
57. Roubidoux, M. A., Kaur, J. S., & Rhoades, D. A. (2022). Health Disparities in Cancer Among American Indians and Alaska Natives. Academic radiology, 29(7), 1013–1021. https://doi.org/10.1016/j.acra.2021.10.011
58. Roubidoux et al., 2022.
59. Roubidoux et al., 2022.
60. Welch, A. C., London, S. M., Wilshire, C. L., Gilbert, C. R., Buchwald, D., Ferguson, G., Allick, C., & Gorden, J. A. (2024). Access to Lung Cancer Screening Among American Indian and Alaska Native Adults: A Qualitative Study. Chest, 165(3), 716–724. https://doi.org/10.1016/j.chest.2023.10.025
61. Tsosie, U., Anderson, N., Woo, N., Dee, C., Echo-Hawk, A., Baker, L., Rusk, A. M., Barrington, W., Parker, M., & Triplette, M. (2024). Understanding determinants of lung cancer preventive care in at-risk urban American Indians and Alaska Natives: A mixed-methods study. Preventive medicine reports, 45, 102822. https://doi.org/10.1016/j.pmedr.2024.102822
62. Kratzer, T. B., Star, J., Minihan, A. K., Bandi, P., Scout, N. F. N., Gary, M., Riddle-Jones, L., Giaquinto, A. N., Islami, F., Jemal, A., & Siegel, R. L. (2024). Cancer in people who identify as lesbian, gay, bisexual, transgender, queer, or gender-nonconforming. Cancer, 130(17), 2948–2967. https://doi.org/10.1002/cncr.35355
63. Monestime, S., Rigney, M., Phipps, N., Carlson, C., Alongi, T., Redding, M., & King, J. C. (2023). Health inequities across the lung cancer care continuum in ten marginalized populations: a narrative review. Journal of thoracic disease, 15(11), 6345–6361. https://doi.org/10.21037/jtd-23-727
64. Monestime et al., 2023.
65. Drysdale, K., Cama, E., Botfield, J., Bear, B., Cerio, R., & Newman, C. E. (2021). Targeting cancer prevention and screening interventions to LGBTQ communities: A scoping review. Health & social care in the community, 29(5), 1233–1248. https://doi.org/10.1111/hsc.13257
66. Monestime et al., 2023.
67. Sahar, L., Douangchai Wills, V. L., Liu, K. K. A., Fedewa, S. A., Rosenthal, L., Kazerooni, E. A., Dyer, D. S., & Smith, R. A. (2022). Geographic access to lung cancer screening among eligible adults living in rural and urban environments in the United States. Cancer, 128(8), 1584–1594. https://doi.org/10.1002/cncr.33996
68. Sahar et al. 2022.
69. Schiffelbein, J. E., Carluzzo, K. L., Hasson, R. M., Alford-Teaster, J. A., Imset, I., & Onega, T. (2020). Barriers, Facilitators, and Suggested Interventions for Lung Cancer Screening Among a Rural Screening-Eligible Population. Journal of primary care & community health, 11, 2150132720930544. https://doi.org/10.1177/2150132720930544
70. Schiffelbein et al. 2020.
71. Centers for Disease Control and Prevention (2024). People With Low Socioeconomic Status Experience a Health Burden From Commercial Tobacco. Retrieved from https://www.cdc.gov/tobacco-health-equity/collection/low-ses-health-burden.html
72. CDC, 2024.
73. CDC, 2024 ; Tailor, T. D., Bell, S., Doo, F. X., & Carlos, R. C. (2023). Repeat Annual Lung Cancer Screening After Baseline Screening Among Screen-Negative Individuals: No-Cost Coverage Is Not Enough. Journal of the American College of Radiology : JACR, 20(1), 29–36. https://doi.org/10.1016/j.jacr.2022.11.005
74. U.S. National Cancer Institute. (2022). Treating smoking in cancer patients: An essential component of cancer care (National Cancer Institute Tobacco Control Monograph 23. U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute. https://cancercontrol.cancer.gov/brp/tcrb/monographs/monograph-23
75. Castro, S., Sosa, E., Lozano, V., Akhtar, A., Love, K., Duffels, J., Raz, D. J., Kim, J. Y., Sun, V., & Erhunmwunsee, L. (2021). The impact of income and education on lung cancer screening utilization, eligibility, and outcomes: a narrative review of socioeconomic disparities in lung cancer screening. Journal of thoracic disease, 13(6), 3745–3757. https://doi.org/10.21037/jtd-20-3281
76. Castro et al., 2021.
77. Castro et al., 2021.