About Melanoma and Skin Cancer Awareness Month
Melanoma and Skin Cancer Awareness Month is an annual opportunity to raise awareness about melanoma and skin cancer, as well as focus on research into their cause, prevention, diagnosis, treatment and survivorship. The goal is to support those affected by melanoma and skin cancer and encourage health-promoting behaviors such as monitoring changes in skin appearance, avoiding indoor tanning and following sun safety practices. According to the Centers for Disease Control and Prevention (CDC), skin cancer is the most common form of cancer in the United States (CDC, 2020). Melanoma and Skin Cancer Awareness Month begins on May 1st and ends on May 31st. The first Monday of May is designated as “Melanoma Monday.” The Friday before Memorial Day is designated as “Don’t Fry Day” to encourage sun safety awareness (National Council on Skin Cancer Prevention, 2019).
Data and Statistics
In 2018, the latest year for which incidence data is available, 83,996 cases of melanoma were reported and 8,199 people died of this cancer in the United States alone (U.S. Cancer Statistics Working Group, 2021). For every 100,000 people, 22 new melanoma cases were reported and two people died of this cancer (U.S. Cancer Statistics Working Group, 2021). Melanoma accounts for the vast majority of skin cancer deaths (American Cancer Society [ACS], 2021).
Current recommendations by the United States Preventive Services Task Force (USPSTF) indicate that the evidence is insufficient to assess the balance of benefits and harms of visual skin examination by a clinician to screen for skin cancer in adults (USPSTF, 2018). However, USPSTF recommends counseling individuals ages six to 24 years, including young adults, adolescents, children and parents of young children with fair skin types, about minimizing ultraviolet (UV) radiation exposure (USPSTF, 2018).
Early detection and prevention continue to be proven tools to reduce the burden of melanoma in the United States. Risk factors like indoor tanning (which significantly increases lifetime risk of melanoma) pose a significant threat. According to the 2019 Youth Risk Behavior Surveillance System, 4.5% of American high schoolers reported using indoor tanning devices, with White high school-aged female students using indoor tanning the most (CDC, 2019). Data from the 2017 National Youth Risk Behavior survey reports that nationwide, 57.2% of high school students reported a sunburn in the previous year (Kann et al., 2018; Holman et al., 2018).
Best Practices for Communicating About Melanoma and Skin Cancer
Messages around melanoma and skin cancer prevention should (1) provide education about risk factors and prevention strategies; (2) highlight the dangers of indoor tanning and correct misinformation about tanning and pro-tan social norms; and (3) emphasize the importance of policy, systems and environmental (PSE) change strategies to reduce the impact of skin cancer and melanoma at the community level. When crafting materials and messages, always consider the health literacy level of your audience and use plain language.
Messages Should…
Provide education about risk factors and prevention strategies
- Emphasize that sun exposure can be risky even when engaging in brief, daily activities such as walking your dog or waiting for the bus. Some people may think about sun safety only when they spend a summer day at the beach or pool (ACS, 2019).
- Avoid promoting sunscreen as the only form of skin sun protection. Combine sunscreen with protective clothing, wide-brimmed hats, sunglasses, and shade (CDC, 2020a).
- Educate your audience about the possible signs and symptoms of melanoma, like the “ABCDE rule” (Asymmetry, Border, Color, Diameter, Evolving) (ACS, 2019a).
- Present information in formats that are clear and easy to understand. People preferred genetic risk information about melanoma to be presented in visuals (Hamilton et al., 2020; Smit et al., 2015).
- Encourage your audience to know their family history, as a family history of melanoma can elevate an individual’s risk for the disease. Knowing family history can motivate one to take steps to reduce their risk of melanoma. (Bowen et al., 2017).
- Inform your audience that for people of color, skin cancer is often diagnosed too late, making it harder to treat (Skin Cancer Foundation, 2021). During routine patient visits, clinicians should be aware that skin cancer can occur in people of color when meeting with patients for regular visits.
- Skin cancer in people of color are often found in less sun-exposed areas of the body (Skin Cancer Foundation, 2021). Encourage these individuals to perform regular full-body skin exams, especially on less sun-exposed areas of the body such as the palms and soles of the feet.
Highlight the dangers of indoor tanning and correct misinformation about tanning and pro-tanning norms
- Emphasize both the costs of engaging in indoor tanning and the benefits of avoiding it. Health communication messages can use either a gain frame (emphasizing the benefits of avoiding risky behaviors), a loss frame (emphasizing the costs of participating in risky behavior) or a balanced frame (emphasizing both gain and loss themes relatively equally). Evidence suggests that both loss- and balanced-framed messages are effective (Mays & Evans, 2017).
- Use graphical images when conveying the dangers of indoor tanning. Warnings about indoor tanning are most effective when they include visuals and loss framing (Hamilton et al., 2020; Mays & Tercyak, 2015).
- Avoid addressing myths associated with tanning and present the preferred message clearly. Referring to myths, such as having a “base tan” protects you against a sunburn or believing that there is no need for sun protection on cloudy days, does not necessarily decrease an individual’s desire to tan (Truong et al., 2021).
- Remind individuals of the people who would approve of them quitting indoor tanning, like parents, friends or romantic partners (Bleakley et al., 2018). Among frequent indoor tanners, one of the reasons for tanning include social acceptance since individuals may be influenced by having friends that use indoor tanning devices (CDC, 2019a).
- Address appearance concerns and psychological effects of tanning associated with feeling more attractive and confident (CDC, 2019a). Highlight the short-term gains of quitting, like saving money and reducing skin damage (Glanz et al., 2019 & Bleakley et al., 2018).
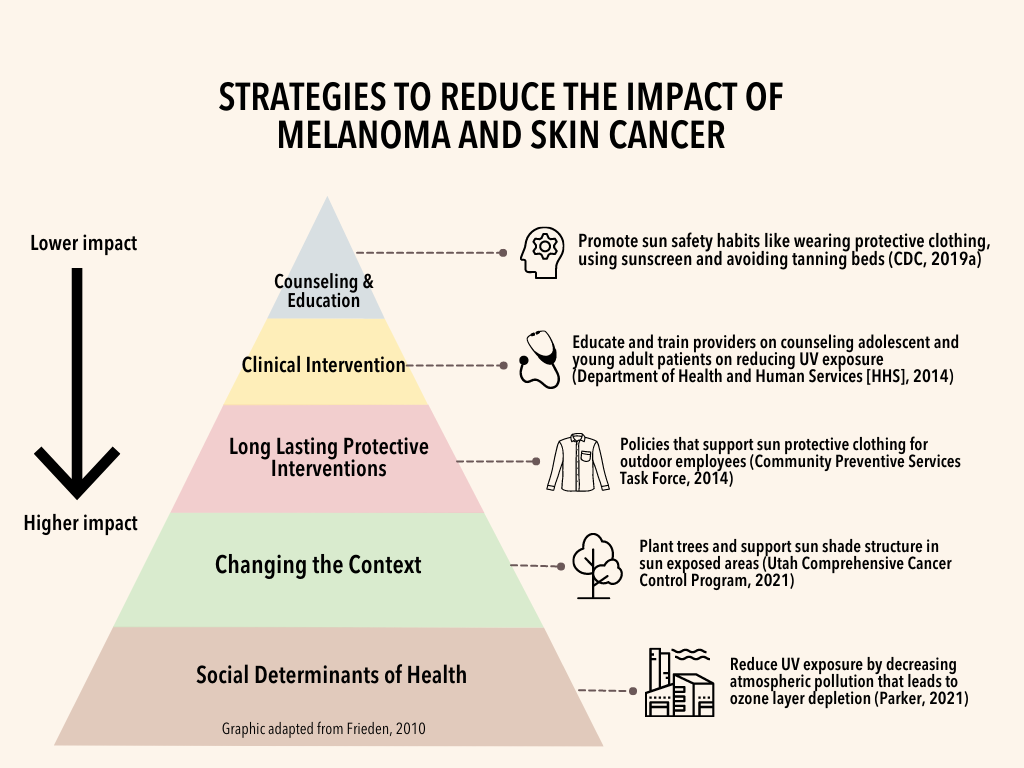
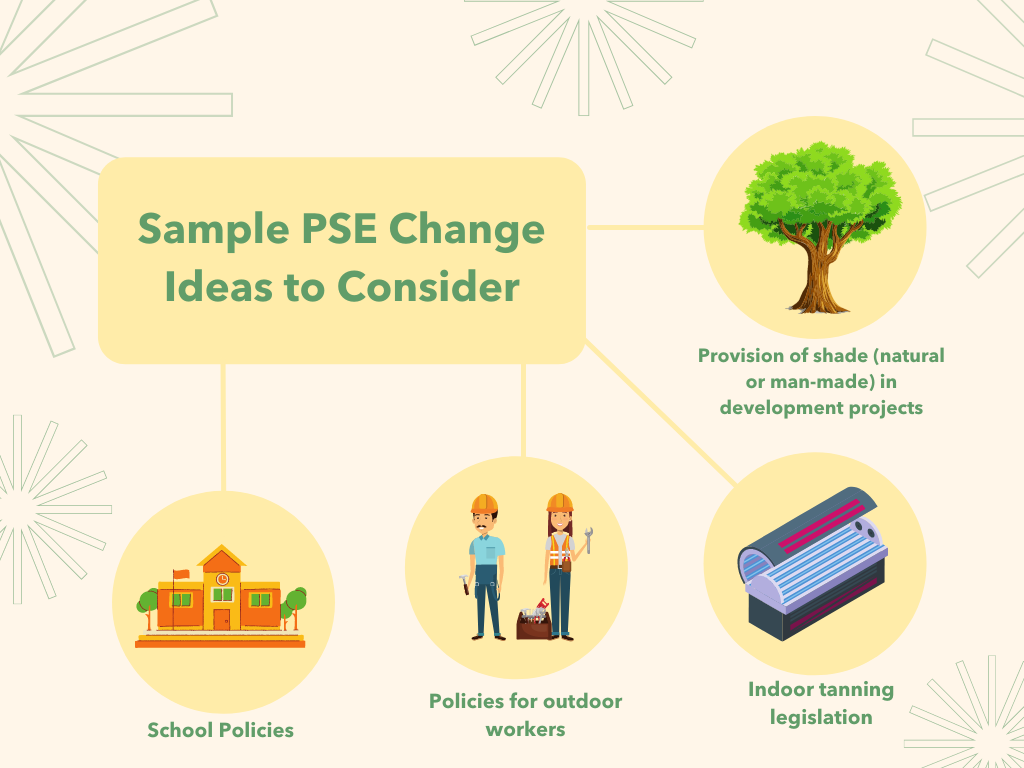
Emphasize the importance of policy, systems and environmental (PSE) change strategies to reduce the impact of melanoma and skin cancer at the community level
- Combine PSE change with a strong communication strategy to make your efforts more effective.
- Explain to your audience why the data is relevant and how it impacts your audience. Use cancer data to inform PSE change efforts (NCI, 2011).
- Engage with other partners like local parks, recreational facilities, clinicians and outdoor community events to promote your efforts. Ensure you are following and communicating with relevant partners and intended audiences on social media.
- Learn from other organizations’ successful interventions to reduce the impact of melanoma and skin cancer. Highlight your organization’s success stories through tools like Action for PSE Change or CDC’s Skin Cancer Prevention Success Stories.
- Focus on community engagement to empower communities to take part in the PSE change process and advocate for their own health. Community-based systematic changes lead to more consistent long-term health improvements than temporary interventions (ACS, 2015).
Communicating with Diverse Audiences
Certain groups experience disparities in melanoma and skin cancer incidence, mortality, and survival (National Cancer Institute, 2020). Cancer health disparities are complex and affected by various factors, such as social determinants of health, behavior, biology, genetics, and more (National Cancer Institute, 2020). Communication-related issues may also play a role in cancer disparities (White-Means and Osmani, 2017). Consider the information most useful to each diverse group.
Below you will find considerations for specific audiences, including: Black/African American, Hispanic/Latinx, Asian Americans, Native Hawaiians and Pacific Islanders [AANHPI], and American Indian/Alaska Native [AI/AN] and LGBTQ individuals.
It is important to tailor communication to these populations of focus with messaging that also addresses conditions where these communities live, learn, work and play, as these factors can impact a wide range of health risks and outcomes (CDC, 2021).
Melanoma and Skin Cancer Resources
| Resource | Description |
| American Academy of Dermatology Association | The American Academy of Dermatology has free education resources to help you spread sun-safety messages and increase public awareness about skin cancer. |
| Basic Information About Skin Cancer | This resource from the CDC includes information on skin cancer, the risks, symptoms, prevention, and treatments. |
| CDC’s Skin Cancer Prevention Success Stories | CDC highlights programs that have found innovative ways to help prevent skin cancer in their communities. |
| CDC’s Melanoma Dashboard | This interactive data visualization tool provides the latest relevant state and county-level data on melanoma incidence and mortality, UV levels, and other relevant data to inform skin cancer prevention efforts at the local level. |
| GW Cancer Center: Action for Policy, Systems, and Environmental (PSE) Change: A Training | This training provides background information on the seven-step PSE change process, stepwise worksheets, a PSE action plan template, real world examples from comprehensive cancer control programs, an extensive resource list and approaches to help grow the PSE change evidence base. |
| GW Cancer Center: Together, Equitable, Accessible, Meaningful (TEAM) Training | This training aims to improve health equity by supporting organizational changes at the systems level. The training will help organizations implement quality improvements to advance equitable, accessible and patient-centered cancer care through improved patient-provider communication, cultural sensitivity, shared decision-making and attention to health literacy. |
| How to SPOT Skin Cancer | This infographic from the American Academy of Dermatology Association can be used to regularly check skin. |
| Moles to Melanoma: Recognizing the ABCDE Features | This resource from the National Cancer Institute has collected photographs of different pigmented skin lesions to help patients and other individuals recognize common moles, atypical moles, and melanomas. |
| National Council on Skin Cancer Prevention | The mission of this organization is to prevent skin cancer through education, advocacy, and raising awareness. |
| Prevention and Control of Skin Cancer | In this resource, the CDC discusses the prevention and control of skin cancer, with particular attention to how we can all help people protect their skin and lives while enjoying the outdoors |
| Preventing Skin Cancer: Community Wide Interventions | These interventions from the Community Preventative Services Task Force seek to increase preventative behaviors within a community by targeting a large part of the population in a defined area. |
| Resources to Share | CDC offers scientifically accurate information about skin cancer in a variety of formats. |
| Skin Cancer Concerns in People of Color: Risk Factors and Prevention | This article raises awareness regarding skin cancers in people of color by providing recommendations to clinicians and the general public for early detection and preventive measures. |
| Skin Cancer Foundation | This organization empowers people to take a proactive approach to daily sun protection by offering educational resources on prevention, skin care information, risk factors, early detection, and treatment. |
| Skin Cancer in People of Color Photo Gallery | This resource shows photographs of different pigmented areas on people of color to help individuals and patients recognize moles, atypical moles, and melanomas. |
| Skin Cancer (Including Melanoma)-Patient Version | Resource provided by the National Cancer Institute that provides an overview of skin cancer, information on treatment, causes and prevention, screening and coping with skin cancer. Also includes the latest on skin cancer research and statistics. |
| Skin Cancer Prevention Progress Report 2019 | The CDC’s fifth annual progress report provides the latest national data on skin cancer, highlights successes, and identifies areas for improvement. |
| Sun Safety Evidence-Based Programs Listing | This list of sun-safety interventions from the Evidence-Based Cancer Control Programs website (formerly RTIPS) is a searchable database of evidence-based cancer control programs that provides program planners and public health practitioners easy and immediate access to: 1) programs tested in a research study, 2) publication(s) of the study findings, and 3) program materials used with a particular study population in a specific setting. |
| The Big See Campaign | The Big See Campaign from the Skin Cancer Foundation aims to inspire you to open your eyes, get to know your skin, look in the mirror and keep these 3 words in mind: NEW, CHANGING or UNUSUAL. |
Melanoma and Skin Cancer Awareness Month Messages and Graphics
| Message | Suggested Graphic |
|---|---|
May is #SkinCancerAwareness month! Kick it off by checking out @CDCgov’s new #MelanomaDashboard for relevant prevention data: https://bit.ly/33mzgRA |  Download Image |
Programs have found many innovative ways to help prevent #skincancer in their communities. Learn more: http://bit.ly/2JhhyFY @CDC_Cancer |  Download Image |
If someone in your family has had #melanoma, you may be at increased risk. Learn about skin cancer risk factors from @CDCgov: https://bit.ly/2WYIstq |  Download Image |
What can you do to reduce your risk of skin cancer, including #melanoma? Get some tips: http://bit.ly/2GPxn6i |  Download Image |
Sunlamps and tanning beds promise a bronzed body year-round, but the UV radiation from these devices poses serious health risks: https://www.fda.gov/radiation-emitting-products/tanning/risks-tanning |  Download Image |
Share your #SunSafeSelfie and join the conversation to raise awareness on sun protection! https://bit.ly/3dzFbIJ |  Download Image |
#DYK community skin cancer prevention programs can prevent future #melanoma cases? Learn more: https://www.cdc.gov/vitalsigns/melanoma-test/index.html |  Download Image |
Exercising or being outside is great, but don’t forget your sun protection! http://bit.ly/2uHWX8a |  Download Image |
#CompCancer professionals: Looking for evidence-based interventions to prevent #melanoma in your community? Check out @theNCI and their Evidence-Based Cancer Control Programs for more info: https://bit.ly/36H483Z
|  Download Image |
The Friday before Memorial Day is “Don’t Fry Day!” Take a moment to make sure you’re protecting yourself against #skincancer & #melanoma: https://bit.ly/3hReC38 |  Download Image |
Schools can play an active role in preventing skin cancers like #melanoma. Here’s how you can get involved: https://bit.ly/34qWnhP |  Download Image |
What are some of the signs of #melanoma? This guide from @CDCgov can help you assess changes in your skin: http://bit.ly/2GSmXTc | 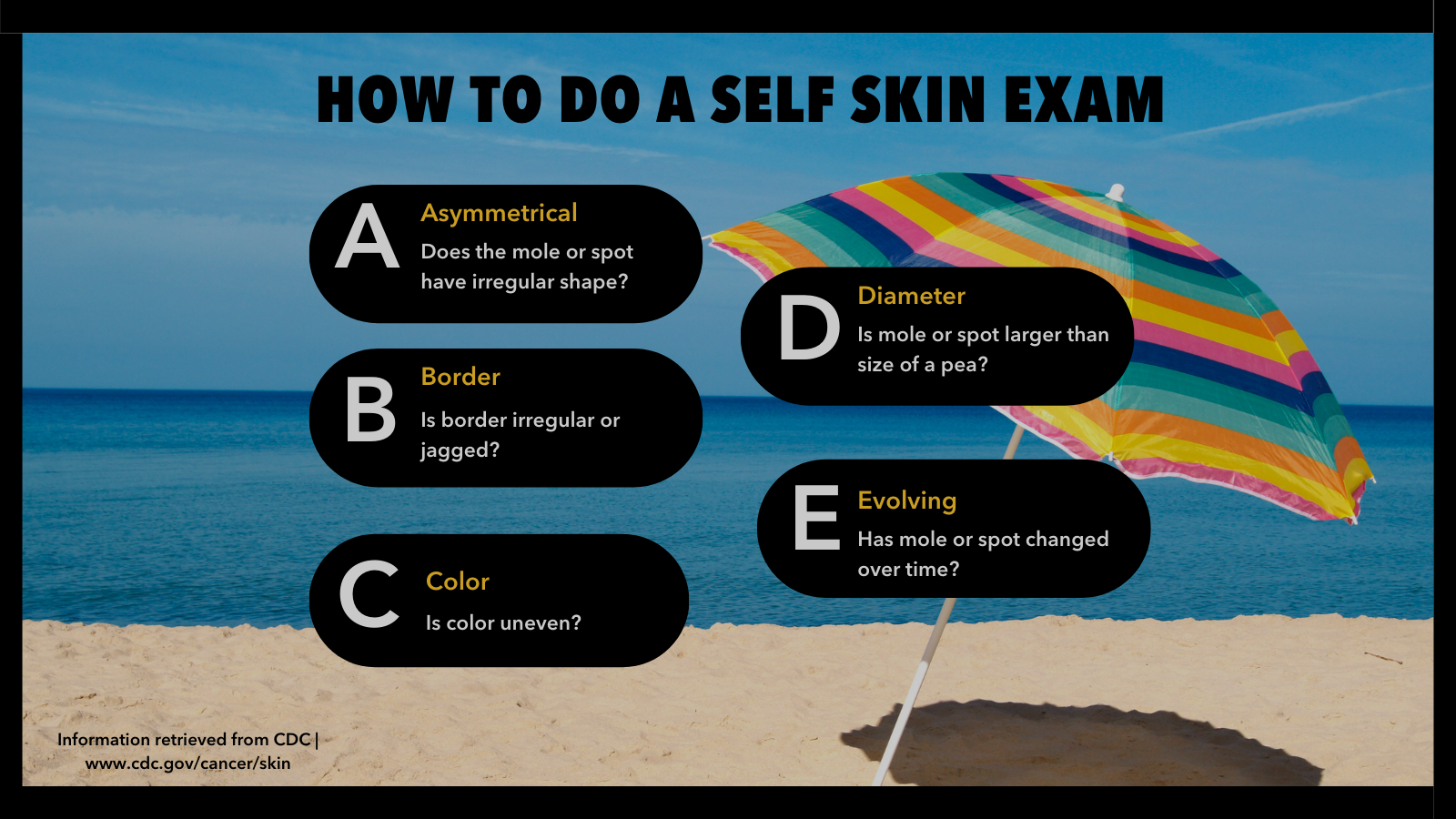 Download Image |
#CompCancer professionals: Looking for PSE change solutions to prevent skin cancer? Start here: https://bit.ly/2Vj04Ob #MelanomaAwareness |  Download Image |
For people of color, when skin cancer develops in non sun- exposed areas, it’s often in a late stage when diagnosed. Luckily, you can find #skincancer early. Check out these tips: https://bit.ly/3dwS59o |  Download Image |
For Black persons, #melanoma can occur in areas that get little sun exposure, like the palms of the hands, soles of the feet, and nail areas. Know the statistics: https://bit.ly/2QTkezv |  Download Image |
In the past two decades, melanoma cases have risen by 20% among Hispanic persons. No one is immune to skin cancer. Get the facts here: https://bit.ly/2QTkezv |  Download Image |
American Indian/Alaska Native persons have the second highest occurrence of melanoma compared to other racial/ethnic groups. Read about indigenous perspectives on skin cancer here: https://bit.ly/3pOkVbU |  Download Image |
#DYK that Asian American, Native Hawaiian and Pacific Islanders can still get skin cancer, even though they are less likely to get sunburned? Check out this infographic: https://bit.ly/3pOV7wv |  Download Image |
#DYK men who identify as gay or bisexual are twice as likely to have skin cancer compared to heterosexual men? Learn more about these disparities: https://bit.ly/3HSuI71 |  Download Image |
Spending more time outdoors during the #COVID19 #pandemic? While summer can be a great time to safely gather for picnics, family reunions and weddings, don’t forget to practice sun safety! Read more: https://bit.ly/3Nj3VF1 |  Download Image |
#COVID19 resulted in delays in diagnosis and treatment of melanoma. Healthcare professionals, here’s how to run your dermatology practice during the pandemic: https://bit.ly/3IZhEym |  Download Image |
#MelanomaMonday is May 2nd this year! Wear your best black attire and head out to spread awareness of #melanoma and #skincancer! Take the time to learn about ways to prevent melanoma: https://bit.ly/36OFNti |  Download Image |
| Message | Suggested Graphic |
|---|---|
| Did you know that May is skin cancer awareness month? Check out CDC’s new #MelanomaDashboard for access to the most recent and relevant data to maximize the impact of our skin cancer prevention efforts: https://bit.ly/33mzgRA |  Download Image |
| Communities across the country are finding innovative ways to reduce the burden of skin cancer and melanoma. Explore their stories and learn more: http://bit.ly/2JhhyFY |  Download Image |
| Did you know that your risk may increase if someone in your family has had melanoma? It’s important to know your family history. For more on skin cancer risk factors: https://bit.ly/2WYIstq |  Download Image |
| What can you do to reduce your risk of skin cancer, including melanoma? Avoid indoor tanning, use sunscreen, and stay in the shade during midday hours: http://bit.ly/2GPxn6i |  Download Image |
| Tanning your skin – in the sun or in a tanning bed – damages your skin. Over time, this damage can lead to prematurely aged skin (e.g., wrinkles and uneven skin color), and, in some cases, skin cancer. |  Download Image |
| Share your #SunSafeSelfie and join the conversation to raise awareness on the benefits of sun protection! https://bit.ly/3dzFbIJ |  Download Image |
| What can you do in your community to help prevent skin cancer? Community-based programs can prevent future cases and lower treatment costs: https://www.cdc.gov/vitalsigns/melanoma-test/index.html |  Download Image |
| Exercising or being outdoors has both physical and mental health benefits. Don’t forget your sunscreen and hat when you’re getting your sweat on with Mother Nature! More tips here: http://bit.ly/2uHWX8a |  Download Image |
| Looking for evidence-based interventions to prevent melanoma and other skin cancers in your community? NCI’s Evidence-Based Cancer Control Programs (EBCCP) is a great place to start: https://bit.ly/36H483Z |  Download Image |
| The Friday before Memorial Day is “Don’t Fry Day!” Help us raise awareness and reduce the rates of skin cancer, including melanoma: https://bit.ly/3hReC38 |  Download Image |
| What can schools do to prevent melanoma and protect students from UV damage? This CDC resource has some practical tips: https://bit.ly/34qWnhP |  Download Image |
| Do you know the ABCDEs of melanoma? This handy guide reminds you to regularly check for changes in your skin and what to look for: http://bit.ly/2GSmXTc | 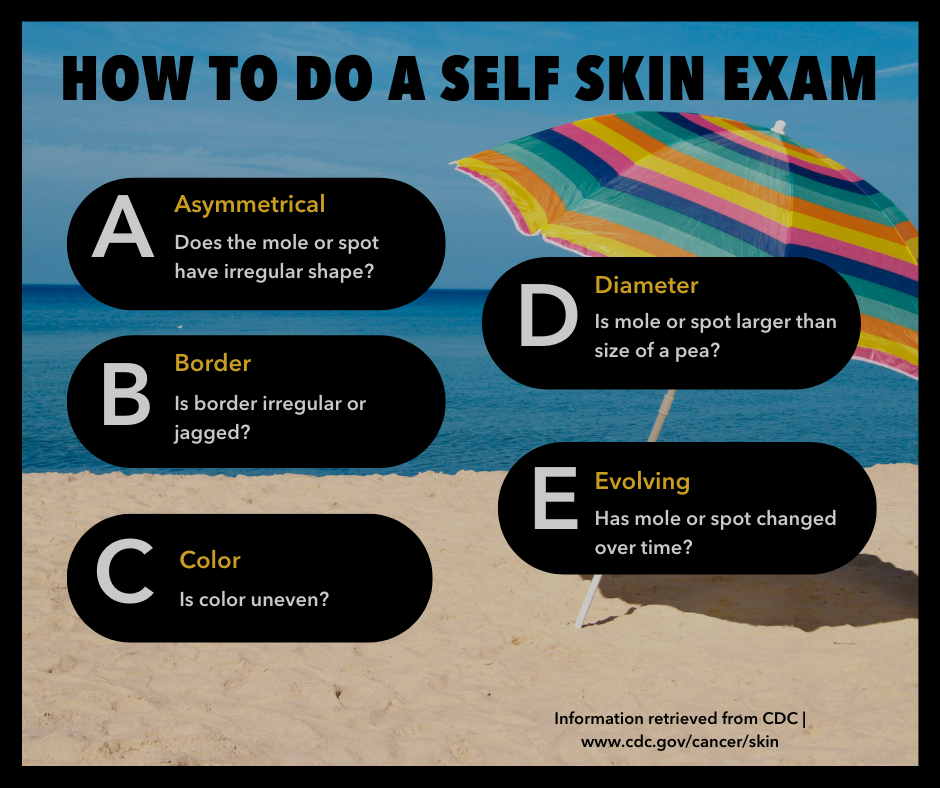 Download Image |
| Comprehensive Cancer Control Professionals: Looking for policy, systems and environmental (PSE) change strategies to prevent skin cancer? Start with the Surgeon General’s Call to Action: https://bit.ly/2Vj04Ob |  Download Image |
| For people of color, when skin cancer develops in non sun-exposed areas, it’s often in a late stage when diagnosed. Luckily, you can find skin cancer early. Check out these tips on how you can look for warning signs: https://bit.ly/3dwS59o |  Download Image |
| For Black persons, #melanoma can occur in areas that get little sun exposure, like the palms of the hands, soles of the feet, and nail areas. Know the statistics: https://bit.ly/2QTkezv | 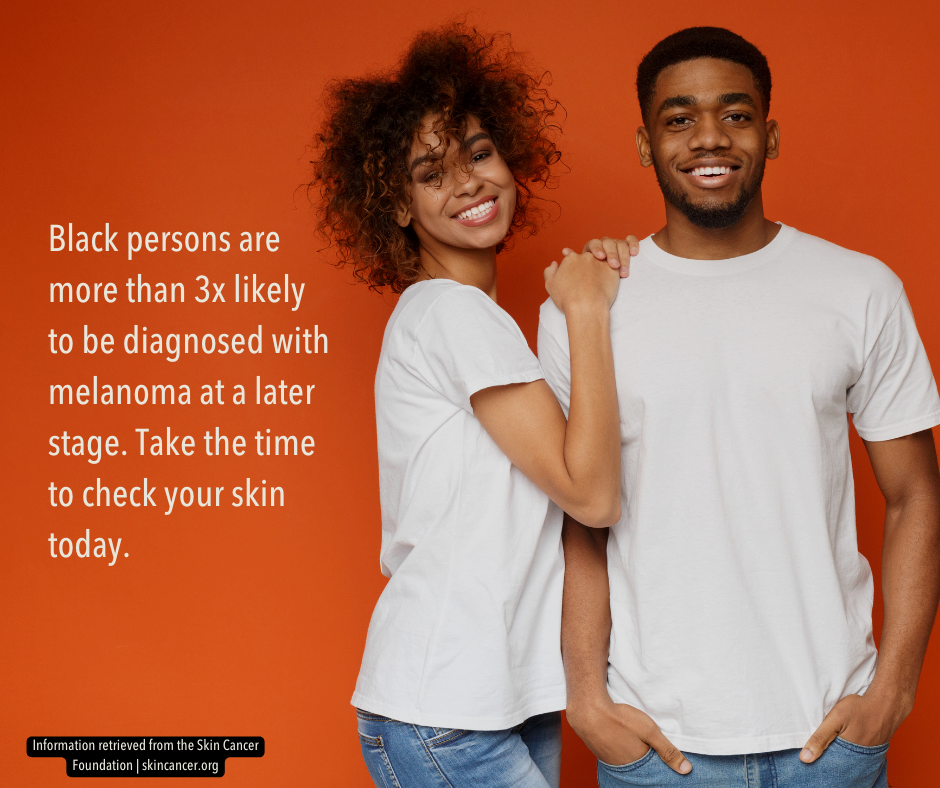 Download Image |
| In the past two decades, melanoma cases have risen by 20% among Hispanic persons. No one is immune to skin cancer. Get the facts: https://bit.ly/2QTkezv |  Download Image |
| American Indian/Alaska Native persons have the second highest occurrence of melanoma compared to other racial/ethnic groups. Read about indigenous perspectives on skin cancer here: https://bit.ly/3pOkVbU |  Download Image |
| Did you know that Asian American, Native Hawaiian and Pacific Islanders can still get skin cancer, even though they are less likely to get sunburned? Check out this infographic here: https://bit.ly/3pOV7wv |  Download Image |
| Did you know that men who identify as gay or bisexual are twice as likely to have skin cancer and six times more likely to use tanning beds compared to heterosexual men? Learn more about these disparities: https://bit.ly/3HSuI71 |  Download Image |
| Spending more time outdoors during the #COVID19 #pandemic? While summer is a great time to safely gather for picnics, family reunions and weddings, don’t forget to practice sun safety! Read more: https://bit.ly/3Nj3VF1 |  Download Image |
| COVID-19 resulted in delays in diagnosis and treatment of melanoma. Healthcare professionals, here’s how to run your dermatology practice during the pandemic: https://bit.ly/3IZhEym |  Download Image |
| #MelanomaMonday is May 2nd this year! Wear your best black attire and head out to spread awareness of #melanoma and #skincancer! Take the time to learn about ways to prevent melanoma: https://bit.ly/36OFNti |  Download Image |
| Message | Suggested Graphic |
|---|---|
| Healthcare Professionals: May is a great time to brush up on current information about skin cancer screening. This summary from the National Cancer Institute provides an overview and description of the evidence: http://bit.ly/2Ya9ZVS |  Download Image |
| Melanoma is one of the top 10 cancers by rates of new cancer cases in the United States. This data visualization tool presents U.S. Cancer Statistics data and demographic trends in an easy-to-understand visual format: http://bit.ly/2KxPy3r |  Download Image |
| May is a great time to spread the word about melanoma and skin cancer prevention with these resources from the Centers for Disease Control and Prevention: https://bit.ly/2QIBLdO |  Download Image |
| Healthcare Professionals: Consider counseling your patients who are at high risk for melanoma -including fair-skinned patients and melanoma survivors -to use sun safety practices: https://bit.ly/2HBZXug |  Download Image |
| Despite the challenges we face during the COVID-19 pandemic, prevention of melanoma and other skin cancers remains a public health priority: https://bit.ly/31ofhAY |  Download Image |
| Message | Suggested Graphic |
|---|---|
| Did you know that May is #skincancer awareness month? Check out @CDCgov’s #MelanomaDashboard for access to the most recent and relevant data to maximize the impact of skin cancer prevention efforts. Visit ephtracking.cdc.gov/Applications/melanomadashboard for more info. |  Download Image |
| Check out @CDCgov’s Skin Cancer Prevention Success stories to learn about innovative ways to reduce the risk of skin cancer in your community. Visit cdc.gov/cancer/skin/success-stories for more info. |  Download Image |
| If someone in your family has had #melanoma, you may be at increased risk. Learn about #skincancer risk factors from @CDCgov. Visit cdc.gov/cancer/skin for more info. |  Download Image |
| What can you do to reduce your risk of #skincancer, including #melanoma? Avoid indoor tanning, use sunscreen, and stay in the shade during midday hours. Visit Visit cdc.gov/cancer/skin for more info. |  Download Image |
| Sunlamps and tanning beds promise a bronzed body year-round, but the UV radiation from these devices poses serious health risks. Visit fda.gov/consumers/consumer-updates/indoor-tanning-risks-ultraviolet-rays for more info. |  Download Image |
| Share your #SunSafeSelfie to raise awareness on the benefits of sun protection! First, photograph yourself using sun protection. Second, post it on social media using the hashtag #SunSafeSelfie. Third, practice what you post! More info at cdc.gov/cancer/skin/sunsafeselfie |  Download Image |
| #DYK community skin cancer prevention programs can prevent future #melanoma cases? Learn more at cdc.gov/vitalsigns/melanoma |  Download Image |
| Exercising or being outside is great, but don’t forget your sun protection! Read more at cdc.gov/cancer/skin on ways to protect your skin from the sun! |  Download Image |
| #CompCancer professionals: Looking for evidence-based interventions to prevent #melanoma in your community? Check out @NationalCancerInstitute’s Evidence-Based Cancer Control Programs (EBCCP) for information on how to get started in your community. Visit ebccp.cancercontrol.cancer.gov for more info! |  Download Image |
| The Friday before Memorial Day is #DontFryDay!” Take a moment to make sure you’re protecting yourself against #skincancer & #melanoma. Check out skincancerprevention.org/get-involved/don’t-fry-day for more info! |  Download Image |
| What can schools do to prevent #melanoma and protect students from #UV damage? This @CDCgov resource has some practical tips at cdc.gov/cancer/skin/what_cdc_is_doing/guidelines |  Download Image |
| Do you know the ABCDEs of #melanoma? This handy guide reminds you to regularly check for changes in your skin and what to look for. Visit cdc.gov/ cancer/skin/basic_info for more info. |  Download Image |
| #CompCancer professionals: Looking for PSE change solutions to prevent skin cancer? Start here: www.hhs.gov/surgeongeneral/reports-and-publications/skin-cancer/consumer-booklet #MelanomaAwareness |  Download Image |
| When skin cancer develops in non sun- exposed areas, it’s often in a late stage when diagnosed. Luckily, you can find #skincancer early. Check out tips from the @aadskin1 on skin cancer in people of color. |  Download Image |
| For Black persons #melanoma can occur in areas that get little sun exposure, like the palms of the hands, soles of the feet, and nail areas. Know the statistics. Visit @skincancerorg for more info. |  Download Image |
| In the past two decades, melanoma cases have risen by 20% among Hispanic persons. No one is immune to skin cancer. Get the facts from the @skincancerorg |  Download Image |
| American Indian/Alaska Native persons have the second highest occurrence of #melanoma compared to other racial/ethnic groups. Promote sun-safety practices in our indigenous communities. Check out @americanindiancancer for more resources. |  Download Image |
| Did you know that Asian American, Native Hawaiian and Pacific Islanders can still get skin cancer, even though they are less likely to get sunburned? Practice sun-safety and do regular skin self-exams. Visit @cdcgov for more guidance on skin cancer prevention. |  Download Image |
| #DYK, men who identify as gay or bisexual are twice as likely to have skin cancer compared to heterosexual men? Visit @lgbtcancernetwork for more resources on skin cancer in the queer community. |  Download Image |
| Spending more time outdoors during the #COVID19 #pandemic? While summer is a great time to safely gather for picnics, family reunions and weddings, don’t forget to practice sun safety! Read more at cdc.gov/cancer/skin |  Download Image |
| #COVID19 resulted in delays in diagnosis and treatment of melanoma. Healthcare professionals, here’s a step-by-step guide on how to run your dermatology practice during COVID-19. Check out aad.org/member/practice/coronavirus/running-your-dermatology-practice |  Download Image |
| #MelanomaMonday is May 2nd this year! Wear your best black attire and head out to spread awareness of melanoma and skin cancer! Information on melanoma prevention here at cdc.gov/cancer/skin |  Download Image |
Download All Messages and Graphics
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets below can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Download All Facebook Messages
Download All LinkedIn Messages
Download All Instagram Messages
If you would like to download all images in this social media toolkit, click on each network below for a zip file with each network’s graphics. Please note that these image sizes are slightly smaller than the links above due to file size limitations. If you would like to download full resolution versions, simply click on the “Download Graphic” link below each image in the message tables above.
Download All Facebook Graphics
Download All LinkedIn Graphics
Download All Instagram Graphics
References
Admassu, N., Pimentel, M. A., Halley, M. C., Torres, J., Pascua, N., Katz, K. A., & Linos, E. (2019). Motivations among sexual-minority men for starting and stopping indoor tanning. The British journal of dermatology, 180(6), 1529–1530. https://doi.org/10.1111/bjd.17684
American Cancer Society. (2015). Policy, systems and environmental change resource guide. Retrieved from https://cancercontroltap.org/policy-systems-and-environmental-change-resource-guide
American Cancer Society. (2019). How do I protect myself from UV rays? Retrieved from https://www.cancer.org/cancer/skin-cancer/prevention-and-early-detection/uv-protection.html
American Cancer Society. (2019a). What should I look for on a skin self-exam? Retrieved from https://www.cancer.org/cancer/skin-cancer/prevention-and-early-detection/what-to-look-for.html
American Cancer Society. (2021). Key Statistics for Melanoma Skin Cancer. Retrieved from https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html
American Cancer Society (2022). Cancer Facts & Figures 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf
American Indian Cancer Foundation (2020). Cancer Plan 2020-2022. https://www.americanindiancancer.org/wp-content/uploads/2020/07/Urban-Cancer-Solutions-Cancer-Plan_-2020-2022-Version_-6_16_2020.pdf
Bleakley, A., Jordan, A., Ellithorpe, M. E., Lazovich, D., Grossman, S., & Glanz, K. (2018). A national survey of young women’s beliefs about quitting indoor tanning: Implications for health communication messages. Translational Behavioral Medicine, 8(6), 898-906. https://academic.oup.com/tbm/article-abstract/8/6/898/4938473?redirectedFrom=fulltext
Bowen, D. J., Albrecht, T., Hay, J., Eggly, S., Harris-Wei, J., Meischke, H., & Burke, W. (2017). Communication among melanoma family members. Journal of Health Communication, 22(3), 198-204. http://dx.doi.org/10.1080/10810730.2016.1259374
Bowers, J.M., Hamilton, J. G., Wu, Y. P., Moyer, A., & Hay, J. L. (2021). Acculturation, Sun Tanning Behavior, and Tanning Attitudes Among Asian College Students in the Northeastern USA. International Journal of Behavioral Medicine, 29(1), 25–35. https://doi.org/10.1007/s12529-021-09993-x
Centers for Disease Control and Prevention. (2019). 1991-2019 High School Youth Risk Behavior Survey Data. Retrieved from https://yrbs-explorer.services.cdc.gov/#/graphs?questionCode=QNINDOORTANNING&topicCode=C08&location=XX&year=2019
Centers for Disease Prevention and Control (2019a). 2019 Skin Cancer Prevention Progress Report. U.S. Department of Health and Human Services. https://stacks.cdc.gov/view/cdc/81911
Centers for Disease Control and Prevention. (2020). Kinds of Cancer. Retrieved from https://www.cdc.gov/cancer/kinds.htm#:~:text=Skin%20cancer%20is%20the%20most%20common%20cancer%20in%20the%20United%20States
Centers for Disease Control and Prevention. (2020a). Sun Safety. Retrieved from https://www.cdc.gov/cancer/skin/basic_info/sun-safety.htm
Centers for Disease Control and Prevention (2021). About Social Determinants of Health (SDOH). Retrieved from https://www.cdc.gov/socialdeterminants/about.html
Centers for Disease Control and Prevention (2021a). What Are the Risk Factors for Skin Cancer? Retrieved from https://www.cdc.gov/cancer/skin/basic_info/risk_factors.htm
Chen, J.M. & Francis-Tan, A. (2021). Setting the Tone: An Investigation of Skin Color Bias in Asia. Race and Social Problems. https://doi.org/10.1007/s12552-021-09329-0
Chen, R., Hipp, J. A., Morrison, L., Henriksen, L., Swetter, S. M., & Linos, E. (2019). Association of Number of Indoor Tanning Salons With Neighborhoods With Higher Concentrations of Male-Male Partnered Households. JAMA Network Open, 2(10), e1912443–e1912443. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2752348
Community Preventive Services Task Force (2014). Preventing Skin Cancer: Interventions in Outdoor Occupational Settings. https://www.thecommunityguide.org/sites/default/files/assets/Skin-Cancer-Outdoor-Occupational-Settings.pdf
Coups, E. J., Stapleton, J. L., Hudson, S. V., Medina-Forrester, A., Rosenberg, S. A., Gordon, M. A., Natale-Pereira, A., & Goydos, J. S. (2013). Linguistic acculturation and skin cancer-related behaviors among Hispanics in the southern and western United States. JAMA dermatology, 149(6), 679–686. doi: 10.1001/jamadermatol.2013.745
Culp M.B., Lunsford N.B. (2019). Melanoma Among Non-Hispanic Black Americans. Prev Chronic Dis 2019;16:180640. DOI: http://dx.doi.org/10.5888/pcd16.180640
Frieden, T. R. (2010). A framework for public health action: The health impact pyramid. American Journal of Public Health, 100(4), 590-595. http://dx.doi.org/10.2105/AJPH.2009.185652
Glanz, K., Jordan, A., Lazovich, D., & Bleakley, A. (2019). Frequent indoor tanners’ beliefs about indoor tanning and cessation. American Journal of Health Promotion, 33(2), 293-299. http://dx.doi.org/10.1177/0890117118784235
Hamilton, J.G., Genoff Garzon, M., Shah, I.H., Cadet, K., Shuk, E., Westerman, J.S., Hay, J.L., Offit, K., & Robson, M.E. (2020). Illustrating Cancer Risk: Patient Risk Communication Preferences and Interest Regarding a Novel BRCA1/2 Genetic Risk Modifier Test. Public health genomics, 23(1-2), 6-19. https://karger.com/phg/article/23/1-2/6/272923/Illustrating-Cancer-Risk-Patient-Risk
Holman, D. M., Ding, H., Guy, G. P. Jr., Watson, M., Hartman, A. M., & Perna, F. M. (2018). Prevalence of sun protection use and sunburn and association of demographic and behavioral characteristics with sunburn among US adults. JAMA Dermatology, 154(5), 561-568. https://stacks.cdc.gov/view/cdc/55069
Idoate, R., Gilbert, M., King, K. M., Spellman, L., McWilliams, B., Strong, B., Bronner, L., Siahpush, M., Ramos, A. K., Clarke, M., Michaud, T., Godfrey, M., & Solheim, J. (2020). Urban American Indian Community Health Beliefs Associated with Addressing Cancer in the Northern Plains Region. Journal of Cancer Education, 36(5), 996–1004. https://doi.org/10.1007/s13187-020-01727-z
Idoate, R., McWilliams, B. & Walsh, S. (2021, May 25). Indigenous Perspectives on Skin Cancer [Webinar]. American Indian Cancer Foundation. https://www.youtube.com/watch?v=eqJQ8QmSQh4
Kann, L., McManus, T., Harris, W. A., Shanklin, S. I., Flint, K. H., Queen, B.,… & Ethier, K. A. (2018). Youth risk behavior surveillance – United States, 2017. Morbidity and Mortality Weekly Report Surveillance Summary, 67(8), 1-479. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6002027/
Kryatova, M.S. and Okoye, G.A. (2016), Dermatology in the North American Indian/Alaska Native population. Int J Dermatol, 55: 125-134. https://doi.org/10.1111/ijd.12977
Lunsford, N.B, Berktold, J., Holman, D. M., Stein, K., Prempeh, A., & Yerkes, A. (2018). Skin cancer knowledge, awareness, beliefs and preventive behaviors among black and hispanic men and women. Preventive medicine reports, 12, 203–209. https://doi.org/10.1016/j.pmedr.2018.09.017
Maarouf, M., Zullo, S. W., DeCapite, T., & Shi, V. Y. (2019). Skin Cancer Epidemiology and Sun Protection Behaviors Among Native Americans. Journal of drugs in dermatology : JDD, 18(5), 420–423. https://pubmed.ncbi.nlm.nih.gov/31141849/
Mansh, M., & Arron, S. T. (2016). Indoor tanning and melanoma: are gay and bisexual men more at risk?. Melanoma management, 3(2), 89–92. https://doi.org/10.2217/mmt-2015-0002
Mansh, M., Katz, K. A., Linos, E., Chren, M. M., & Arron, S. (2015). Association of Skin Cancer and Indoor Tanning in Sexual Minority Men and Women. JAMA dermatology, 151(12), 1308–1316. https://jamanetwork.com/journals/jama/fullarticle/2779985
Mays, D. & Evans, W.D. (2017). The effects of gain-, loss-, and balanced-framed messages for preventing indoor tanning among young adult women. Journal of Health Communication, 22(7): 604–611. http://dx.doi.org/10.1080/10810730.2017.1332119
Mays, D. & Tercyak, K. P. (2015). Framing indoor tanning warning messages to reduce skin cancer risks among young women: Implications for research and policy. American Journal of Public Health, 105(8), e70-e76. http://dx.doi.org/10.2105/AJPH.2015.302665
Melanoma Research Alliance (n.d.). Melanoma & Skin of Color. https://www.curemelanoma.org/about-melanoma/people-of-color/
National Cancer Institute. (2020). Cancer disparities. Retrieved August 11, 2021 from https://www.cancer.gov/about-cancer/understanding/disparities
National Cancer Institute. (2011). Making data talk: A workbook. Retrieved from https://www.cancer.gov/publications/health-communication/making-data-talk.pdf
National Council on Skin Cancer Prevention. (2019). Don’t fry day [webpage]. Retrieved from https://www.skincancerprevention.org/programs/dont-fry-day
Niu, Z.; Riley, M.; Stapleton, J.L.; Ochsner, M.; Hernandez, G.; Kimmel, L.; Giovenco, D.P.; Hudson, S.V.; O’Malley, D.; Lozada, C.; et al. (2022). Sunburns and Sun Protection Behaviors among Male Hispanic Outdoor Day Laborers. Int. J. Environ. Res. Public Health, 19, 2524. https://doi.org/10.3390/ijerph19052524
Parker, E.R. (2021). The influence of climate change on skin cancer incidence – A review of the evidence. International Journal of Women’s Dermatology, 7(1), 17–27. https://doi.org/10.1016/j.ijwd.2020.07.003
Perez M. I. (2019). Skin Cancer in Hispanics in the United States. Journal of drugs in dermatology : JDD, 18(3), s117–s120. https://pubmed.ncbi.nlm.nih.gov/30909356/
Ragan, K.R., Buchanan Lunsford, N., Thomas, C. C., Tai, E. W., Sussell, A., & Holman, D. M. (2019). Skin Cancer Prevention Behaviors Among Agricultural and Construction Workers in the United States, 2015. Preventing Chronic Disease, 16, E15–E15. https://doi.org/10.5888/pcd16.180446
Schwarz, N., Sanna, L. J., Skurnik, I., & Yoon, C. (2007). Metacognitive experiences and the intricacies of setting people straight: Implications for debiasing and public information campaigns. Advances in Experimental Social Psychology, 39, 127-161. https://doi.org/10.1016/S0065-2601(06)39003-X
Scout, N.F.N. & Rhoten, B. (2021) OUT: The National Cancer Survey, Summary of Findings. National LGBT Cancer Network. https://cancer-network.org/wp-content/uploads/2021/06/OUT-LGBTCancerNetwork-SurveyReport_Final.pdf (PDF)
Singer, S., Tkachenko, E., Hartman, R. I., & Mostaghimi, A. (2020). Association Between Sexual Orientation and Lifetime Prevalence of Skin Cancer in the United States. JAMA dermatology, 156(4), 441–445. https://doi.org/10.1001/jamadermatol.2019.4196
Skin Cancer Foundation. (2021). Skin Cancer & Skin of Color: What you Need to Know. Retrieved from https://www.skincancer.org/skin-cancer-information/skin-cancer-skin-of-color/#stats
Smit, A.K., Keough, L.A., Hersch, J., Newson, A.J., Butow, P., Ed, D.,…, Cust, A.E. (2015). Public preferences for communicating personal genomic risk information: A focus group study. Health Expectations [Published online first]. http://dx.doi.org/10.1111/hex.12406
Supapannachart, K.J., Chen, S. C., Wang, Y., & Yeung, H. (2022). Skin Cancer Risk Factors and Screening Among Asian American Individuals. JAMA Dermatology (Chicago, Ill.). https://jamanetwork.com/journals/jamadermatology/fullarticle/2788388
Truong, A., Forbes, B., Zhang, M., McFadden, M., & Klein, S. (2021). A sun safety pilot program utilizing a tanning myths-focused video contest for Utah adolescents: A cross-sectional analysis (Preprint). JMIR Dermatology. https://doi.org/10.2196/20192
U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention (2021). United States Cancer Statistics Working Group, U.S. Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999-2018). https://gis.cdc.gov/Cancer/USCS/DataViz.html.
U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention (2021a). United States Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999-2018): American Indian and Alaska Native restricted to PRCDA only. Retrieved from https://www.cdc.gov/cancer/uscs/about/tools/AIAN-incidence-analytic-db.htm
U.S. Cancer Statistics Working Group (2021b). U.S. Cancer Statistics Data Visualizations Tool, based on 2020 submission data (1999-2018): Leading Cancers by Age, Sex, Race, and Ethnicity. Retrieved from https://gis.cdc.gov/Cancer/USCS/#/Demographics/
U.S. Department of Health and Human Services (2014). The Surgeon General’s Call to Action to Prevent Skin Cancer. https://www.hhs.gov/sites/default/files/call-to-action-prevent-skin-cancer.pdf
U.S. Preventive Services Task Force (2018). Skin Cancer Prevention: Behavioral Counseling. https://uspreventiveservicestaskforce.org/uspstf/recommendation/skin-cancer-counseling
Utah Comprehensive Cancer Control Program. (2021). 2021–2025 Utah Comprehensive Cancer Prevention and Control Plan. https://ftp.cdc.gov/pub/publications/cancer/ccc/utah-ccc-plan-508.pdf
Watson, M., Holman, D., Fox, K. A., Guy, G. P., Seidenberg, A. B., Sampson, B. P. …Lazovich, D. (2013). Preventing skin cancer through reduction of indoor tanning: Current evidence. American Journal of Preventive Medicine, 44(6), 682-689. http://dx.doi.org/10.1016/j.amepre.2013.02.015
White-Means, S., and Osmani, A. R. (2017). Racial and ethnic disparities in patient-provider communication with breast cancer patients: Evidence from 2011 MEPS and experiences with cancer supplement. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 54, 1-17. https://doi.org/10.1177/0046958017727104
Zheng, Y.J., Ho, C., Lazar, A., & Ortiz-Urda, S. (2021). Poor melanoma outcomes and survival in Asian American and Pacific Islander patients. Journal of the American Academy of Dermatology, 84(6), 1725–1727. https://doi.org/10.1016/j.jaad.2020.08.086

