We would like to acknowledge and thank our co-branding partners for their contributions to this project:
We also extend our gratitude and thanks to our advising partners for their guidance and support:
- Shannon Kozlovich, The National LGBTQI+ Cancer Network
- Priya Raman, Asian Pacific Partners for Empowerment, Advocacy, & Leadership (APPEAL)
About Breast Cancer Awareness Month
National Breast Cancer Awareness Month is recognized each October to raise awareness about the importance of early detection and access to timely, high-quality care for breast cancer. Breast cancer is the most common cancer among females in the U.S., accounting for 32% of newly diagnosed cancers.[1] This toolkit can assist your organization and partners in sharing important information with your networks for breast cancer awareness month.
Data and Statistics
As of 2021, the latest year in which comprehensive data is available, 272,454 new breast cancers were reported in the U.S.[2] The CDC reports that in 2022, 42,211 females died from breast cancer.*[3] Because of health service disruptions throughout 2020 and 2021 due to the COVID-19 pandemic, breast cancer screening, diagnosis, and central cancer registry reporting may be delayed, and actual cancer occurrence may be underreported.
| *Note about terminology: Here we report statistics the way in which they are reported in our source references, while emphasizing their limitations. Data are currently reported as binary sex data (male or female) and ignore gender and sex characteristic differences that make up the intersex spectrum, making it difficult to explain differences across gender and sexual orientations. While the latest North American Association of Central Cancer Registries (NAACCR) data dictionary includes multiple options beyond sex variables, the field may be underused or underreported. We advocate for systematic collection of sex assigned at birth, gender identity, sexual orientation, and intersex status to inform and advance evidence-based guidelines. |
Best Practices for Communicating About Breast Cancer
Promote patient-provider discussions of family history and risk
- Present personalized information about breast cancer risk, especially for individuals at high risk due to family history (primarily first degree relatives).[4]
- Encourage patients to ask questions and disseminate relevant resources to facilitate shared decision-making.[5]
- Encourage providers to emphasize screening, risk reduction, and family history, especially for those at higher risk.
- Remind providers to account for a variety of factors during the shared decision-making process and throughout patient-provider engagement, including lower levels of literacy and health literacy and variations in technology access and digital literacy.[6]
- Acknowledge historical medical biases and promote culturally competent care.
| Use gender-neutral language, when possible. Current data is collected on reported sex (based on only two options: male or female) and does not necessarily correlate with the gender identity of those affected by cancer. Ensure language is inclusive; reflect the words used by your patients to refer to themselves as terminology evolves and varies across communities. |
Encourage screening and screening support for diverse audiences
- Promote routine health checkups to improve adherence to breast cancer screening guidelines.
- Address persistent disparities by providing tailored support for Black, Indigenous, and People of Color (BIPOC), Hispanic individuals and those from racial, ethnic and national backgrounds disproportionately affected by cancer.[7]
- Support provider education onbreast cancer screening guidelines for transgender and nonbinary persons based on American College of Radiology guidelines, and the importance of inclusive communication to reduce care delays and discrimination.[8]
Special recommendations for Health Care Professionals:
Communicate using clear, plain language that supports patient understanding and ability to use health information
- Provide culturally and linguistically appropriate, patient-centered care by acknowledging social stigma and correcting misinformation associated with a breast cancer diagnosis and breast cancer screening (for example, cancer fatalism).[9]
- Create opportunities for patient-initiated questions or concerns and check for understanding.[10]
- Explore a full range of surgical and post-surgical options; have frequent conversations soon after diagnosis for patients to weigh treatment options and make decisions about breast reconstruction.[11]
Share information about long-term care and survivorship
- Promote tailored resources, such as individualized long-term and late effects information and care or information specific to young breast cancer survivors.
- Address sexual and reproductive health needs by asking early about side-effects or concerns and sharing resources to manage long-term side effects.[12]
- Address psychosocial and long term needs of survivors by providing resources and referrals proactively and individually, including specific cancer support groups or mental health resources based on age, gender, or sexual orientation, when available.[13]
- Normalize the need for support. For example, providers can prompt, “We expect that this recovery will be difficult physically and emotionally. How can we help you cope with the physical and emotional aftereffects of cancer?”[14]
- Continue lifelong learning with resources like the American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline; the GW Cancer Survivorship educational offerings and guidelines from the National Comprehensive Cancer Network.
Communicating with Diverse Audiences
Gaps in cancer control engagement and practices contribute to breast cancer outcome disparities.[15] Cancer health disparities are affected by social and political determinants of health, behavior, genetics, provider bias and learned behaviors, as well as lack of tailored guidance for patients.[16] Black and Hispanic or Latine individuals in the US experience disparities in breast cancer screening, incidence, mortality, and survival as a result of systemic inequities.[17] Some individuals experience multiple forms of marginalization in and throughout health systems. This compounded experience of disadvantage may be referred to as intersectionality.
Toolkit Glossary
This section is to support our learners in understanding our toolkit language.
| Intersectionality | A framework for understanding how various forms of social stratification, such as race, gender, class, and sexual orientation, intersect to create unique dynamics and effects of discrimination or privilege. |
| Latine | A gender-neutral term used to refer to people of Latin American descent, offering an inclusive alternative to Latino/Latina. |
| LGBTQI+ | An acronym that stands for Lesbian, Gay, Bisexual, Transgender, Queer or Questioning, and Intersex, with the “+” representing other non-mainstream sexual and gender identities. |
Breast Cancer Resources
| Resource | Description |
|---|---|
| American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline | This breast cancer survivorship care guideline provides recommendations for surveillance for recurrence, screening for second primary cancers, assessment and management of physical and psychosocial long‐term and late effects of breast cancer and its treatment, health promotion, and care coordination/practice implications. |
| Black Women & Breast Cancer: Facts to Know | This fact sheet from the African American Breast Cancer Alliance contains information and resources about breast cancer for Black women. |
| Breast Cancer During Pregnancy | This fact sheet covers common concerns and questions about breast cancer during pregnancy and possible treatment options. |
| Breast Cancer: What Are the Risk Factors? | This CDC web page details risk factors for breast cancer that can and cannot be changed. |
| Breast Self-Awareness Messages for the Black Community | This resource highlights the four key messages of breast self-awareness — know your risk, get screened, know what’s normal for you, and make healthy lifestyle choices. It also shows breast changes that should be reported to a doctor. |
| Cancer Survivorship Education from the GW Cancer Center | GW Cancer Center offers education on cancer survivorship care for clinicians. See the lesson: Breast Cancer Survivorship: Clinical Follow-Up Care Guideline for Primary Care Providers. |
| CDC National Breast and Cervical Cancer Early Detection Program | The CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP) provides free breast and cervical cancer screenings and diagnostic services to low-income people and to those who are uninsured or underinsured (lack adequate comprehensive healthcare coverage). |
| Communicating with your breast cancer care team as an LGBTQI+ person | This short guide helps patients make an informed choice about coming out to their health care team. It provides tips on talking about sexual orientation and gender identity with health care professionals, offers personal stories of people who have come out while coping with a breast cancer diagnosis, and provides advice on how to determine if a treatment center is affirming. |
| Datos Para La Vida | This webpage lists all of Susan G. Komen’s downloadable resources in Spanish separated into sections by type of resource and breast cancer topic. |
| Equitas Health Institute Breast/Chest Guide | This guide contains information and resources about breast and chest health. |
| Fast Facts: Breast Cancer and Financial Barriers | This fact sheet from SelfMade Health Network covers financial challenges associated with breast cancer. |
| Frankly: Conversations about Sex Throughout the Cancer Journey: | This resource shares stories about sex and sexuality throughout LGBTQI+ individuals’ cancer journeys. |
| Genetic Testing and Breast Cancer: Unlocking Family Secrets | This resource highlights the importance of genetic testing in the Black community and how people can find out if genetic testing is right for them. |
| Let’s Talk About Breast Cancer Shareable Images | These images from SelfMade Health Network focus on breast cancer screening. |
| LGBTQI+ Guide for Cancer Screening | This resource creates a personalized guide for LGBTQI+ individuals cancer screening. |
| National LGBTQI+ Cancer Network Shareable Images: Chest/Breast Cancer Screenings in Trans Communities | These images from the National LGBTQI+ Cancer Network promote chest/breast cancer screenings in people of transgender experience. |
| National LGBTQI+ Cancer Network Shareable Images: Delays in Cancer Care | These images from the National LGBTQI+ Cancer Network address delays in cancer care experienced by Black lesbian, gay, and bisexual women. |
| Young Black Women Talk About Breast Cancer | This tri-fold brochure, for use in the U.S., provides awareness messages and general facts about breast cancer in young women, personal stories, and images of young Black breast cancer survivors. |
| Your Breast Cancer Surgery Program | This program has been developed by the American College of Surgeons along with the Commission on Cancer (COC) and the National Accreditation Program for Breast Centers (NAPBC) to support surgical preparation and optimal recovery. |
Social Media Graphics and Captions
| Message | Suggested Graphic |
|---|---|
| October is #BreastCancer Awareness Month! Did you know breast cancer is one of the most common cancers in the U.S.? Read more quick facts: https://bit.ly/3z2fBdb #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk to your doctor to review your family history and ways to reduce your #breastcancer risk. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Locate a #breastcancer screening provider near you. Find out if you qualify for a free or low-cost mammogram through @cdcgov National Breast and Cervical Cancer Early Detection Program: https://bit.ly/4dUwTYB #TAPintoCancerControl #gwccTAP #TAPforBreastCancer | 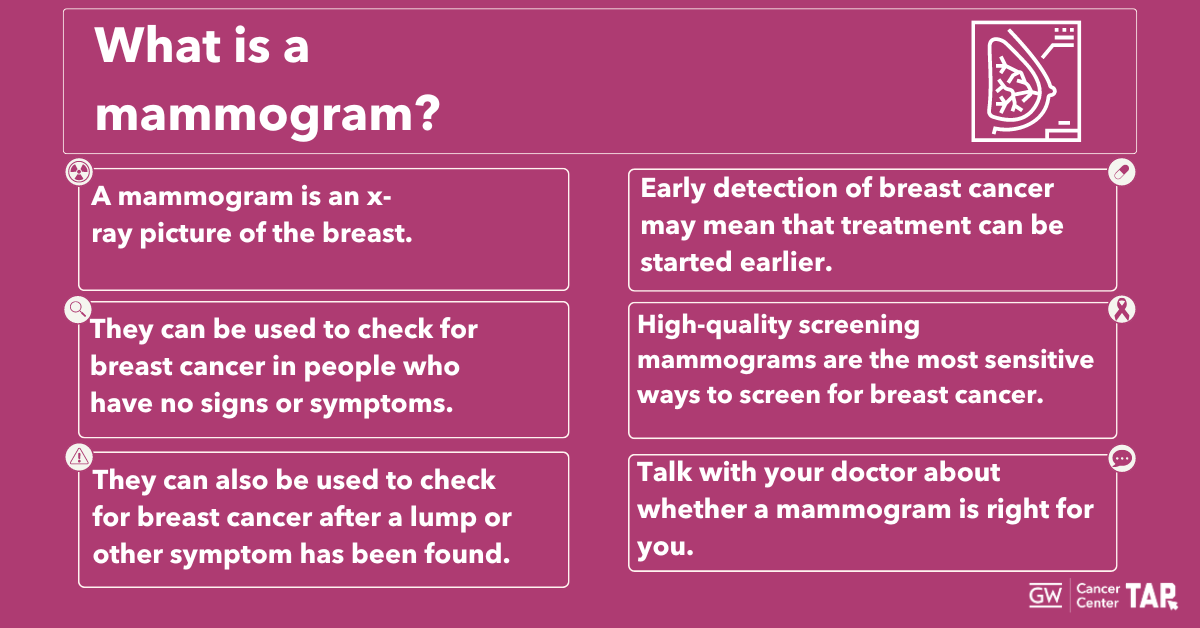 Download Image |
| #Breastcancer clinical trials are critical to improving treatment and creating guidelines for care. Talk to your doctor about whether a trial is right for you @TheNCI’s site: http://bit.ly/329Hhq7 #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| GW offers no-cost training for health professionals on the long-term needs of cancer survivors, including a lesson on #breastcancer. Visit https://bit.ly/3XCKsX0 to learn more. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your breast cancer screening options. Knowing when to start and how often to get screened can make a big difference. #ScreeningSavesLives #BreastHealth #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Did you know that new guidelines from the U.S. Preventive Services Task Force now recommends screening mammography every other year for individuals 40 years old and older? Are you up to date? #ScreeningSavesLives #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Under 45? 1 in 10 patients are diagnosed with breast cancer when they are younger than 45. Learn about risk factors, symptoms of breast cancer in young people, and support to get screened: https://bit.ly/35rdmyS #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Breast cancer affects everyone. It’s important for LGBTQI+ folks to get screened regularly. Talk to your healthcare provider about your risk and screening options. #LGBTQHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Discuss screening options with your healthcare provider today. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Talk with your family about your health history and schedule an appointment with your healthcare provider today! #CancerScreening #ScreeningSavesLives #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Access valuable breast cancer resources in Spanish! Explore @Susan G. Komen’s downloadable resources tailored for the Hispanic community: https://bit.ly/3MHv8lL #HispanicHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer as an LGBTQI+ individual? This guide helps LGBTQI+ folks find access and information to breast and chest health. Find support here: https://bit.ly/3AYAnuK #LGBTQHealth #BreastCancerAwareness @Equitas.Health #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer can be intimidating for everyone. To get accurate and up-to-date information for your #breastcancer questions, talk to your healthcare provider and get support at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| The @nationalcancerinstitute Cancer Information Service can provide accurate, up-to-date, and reliable information for a range of #breastcancer questions. Learn more at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Delaying that mammogram because it may cost too much? There is help! Don’t assume you won’t qualify. Check out your state/tribe/territory program: https://bit.ly/3XcDF4Y #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Recently diagnosed with #breastcancer? The @NationalCancerInstitute has helpful information on treatment, research, and coping with cancer. Learn more by visiting cancer.gov/types/breast. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| October is Breast Cancer Awareness Month! Early detection saves lives. Schedule your mammogram today! #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| It’s Breast Cancer Awareness Month! Talk to your healthcare provider about getting screened today. #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Message | Suggested Graphic |
|---|---|
| October is #BreastCancer Awareness Month! Did you know breast cancer is one of the most common cancers in the U.S.? Read more quick facts: https://bit.ly/3z2fBdb #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk to your doctor to review your family history and ways to reduce your #breastcancer risk. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Locate a #breastcancer screening provider near you. Find out if you qualify for a free or low-cost mammogram through @cdcgov National Breast and Cervical Cancer Early Detection Program: https://bit.ly/4dUwTYB #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| #Breastcancer clinical trials are critical to improving treatment and creating guidelines for care. Talk to your doctor about whether a trial is right for you @TheNCI’s site: http://bit.ly/329Hhq7 #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| GW offers no-cost training for health professionals on the long-term needs of cancer survivors, including a lesson on #breastcancer. Visit https://bit.ly/3XCKsX0 to learn more. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your breast cancer screening options. Knowing when to start and how often to get screened can make a big difference. #ScreeningSavesLives #BreastHealth #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Did you know that new guidelines from the U.S. Preventive Services Task Force now recommends screening mammography every other year for individuals 40 years old and older? Are you up to date? #ScreeningSavesLives #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Under 45? 1 in 10 patients are diagnosed with breast cancer when they are younger than 45. Learn about risk factors, symptoms of breast cancer in young people, and support to get screened: https://bit.ly/35rdmyS #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Breast cancer affects everyone. It’s important for LGBTQI+ folks to get screened regularly. Talk to your healthcare provider about your risk and screening options. #LGBTQHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Discuss screening options with your healthcare provider today. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Talk with your family about your health history and schedule an appointment with your healthcare provider today! #CancerScreening #ScreeningSavesLives #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Access valuable breast cancer resources in Spanish! Explore @Susan G. Komen’s downloadable resources tailored for the Hispanic community: https://bit.ly/3MHv8lL #HispanicHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer as an LGBTQI+ individual? This guide helps LGBTQI+ folks find access and information to breast and chest health. Find support here: https://bit.ly/3AYAnuK #LGBTQHealth #BreastCancerAwareness @Equitas.Health #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer can be intimidating for everyone. To get accurate and up-to-date information for your #breastcancer questions, talk to your healthcare provider and get support at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| The @nationalcancerinstitute Cancer Information Service can provide accurate, up-to-date, and reliable information for a range of #breastcancer questions. Learn more at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Delaying that mammogram because it may cost too much? There is help! Don’t assume you won’t qualify. Check out your state/tribe/territory program: https://bit.ly/3XcDF4Y #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Recently diagnosed with #breastcancer? The @NationalCancerInstitute has helpful information on treatment, research, and coping with cancer. Learn more by visiting cancer.gov/types/breast. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| October is Breast Cancer Awareness Month! Early detection saves lives. Schedule your mammogram today! #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| It’s Breast Cancer Awareness Month! Talk to your healthcare provider about getting screened today. #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Message | Suggested Graphic |
|---|---|
| October is #BreastCancer Awareness Month! Did you know breast cancer is one of the most common cancers in the U.S.? Read more quick facts: https://bit.ly/3z2fBdb #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk to your doctor to review your family history and ways to reduce your #breastcancer risk. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Locate a #breastcancer screening provider near you. Find out if you qualify for a free or low-cost mammogram through @cdcgov National Breast and Cervical Cancer Early Detection Program: https://bit.ly/4dUwTYB #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| #Breastcancer clinical trials are critical to improving treatment and creating guidelines for care. Talk to your doctor about whether a trial is right for you @TheNCI’s site: http://bit.ly/329Hhq7 #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| GW offers no-cost training for health professionals on the long-term needs of cancer survivors, including a lesson on #breastcancer. Visit https://bit.ly/3XCKsX0 to learn more. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your breast cancer screening options. Knowing when to start and how often to get screened can make a big difference. #ScreeningSavesLives #BreastHealth #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Did you know that new guidelines from the U.S. Preventive Services Task Force now recommends screening mammography every other year for individuals 40 years old and older? Are you up to date? #ScreeningSavesLives #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Under 45? 1 in 10 patients are diagnosed with breast cancer when they are younger than 45. Learn about risk factors, symptoms of breast cancer in young people, and support to get screened: https://bit.ly/35rdmyS #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Breast cancer affects everyone. It’s important for LGBTQI+ folks to get screened regularly. Talk to your healthcare provider about your risk and screening options. #LGBTQHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Discuss screening options with your healthcare provider today. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Talk with your family about your health history and schedule an appointment with your healthcare provider today! #CancerScreening #ScreeningSavesLives #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Access valuable breast cancer resources in Spanish! Explore @Susan G. Komen’s downloadable resources tailored for the Hispanic community: https://bit.ly/3MHv8lL #HispanicHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer as an LGBTQI+ individual? This guide helps LGBTQI+ folks find access and information to breast and chest health. Find support here: https://bit.ly/3AYAnuK #LGBTQHealth #BreastCancerAwareness @Equitas.Health #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer can be intimidating for everyone. To get accurate and up-to-date information for your #breastcancer questions, talk to your healthcare provider and get support at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| The @nationalcancerinstitute Cancer Information Service can provide accurate, up-to-date, and reliable information for a range of #breastcancer questions. Learn more at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer | 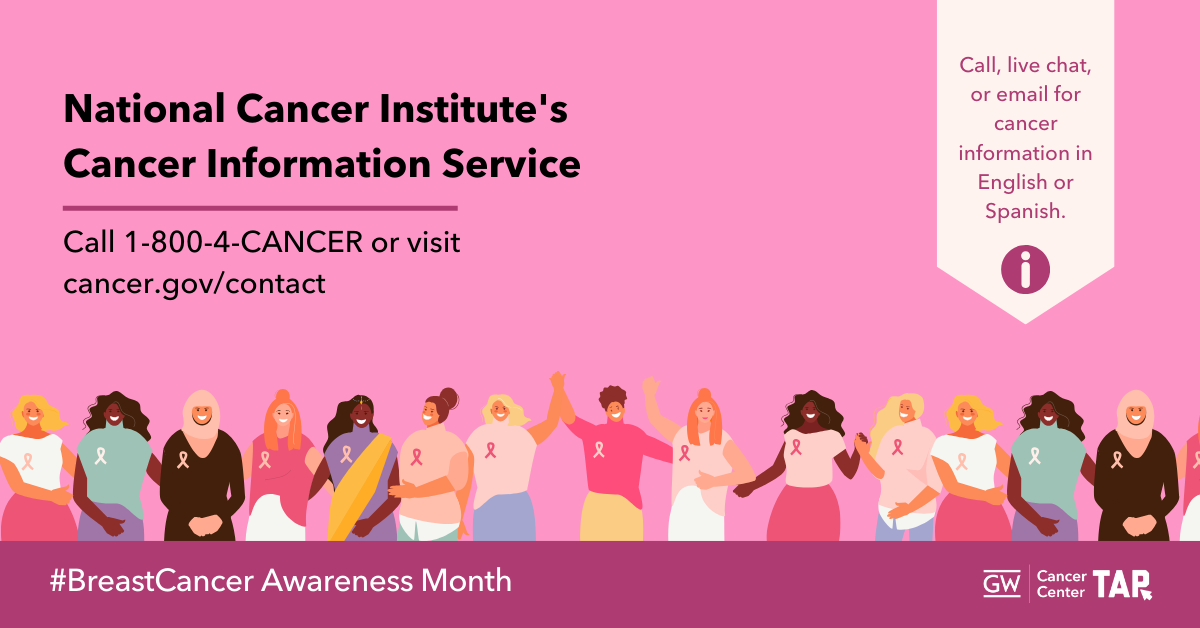 Download Image |
| Delaying that mammogram because it may cost too much? There is help! Don’t assume you won’t qualify. Check out your state/tribe/territory program: https://bit.ly/3XcDF4Y #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Recently diagnosed with #breastcancer? The @NationalCancerInstitute has helpful information on treatment, research, and coping with cancer. Learn more by visiting cancer.gov/types/breast. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| October is Breast Cancer Awareness Month! Early detection saves lives. Schedule your mammogram today! #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| It’s Breast Cancer Awareness Month! Talk to your healthcare provider about getting screened today. #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Message | Suggested Graphic |
|---|---|
| October is #BreastCancer Awareness Month! Did you know breast cancer is one of the most common cancers in the U.S.? Read more quick facts: https://bit.ly/3z2fBdb #TAPintoCancerControl #gwccTAP #TAPforBreastCancer | 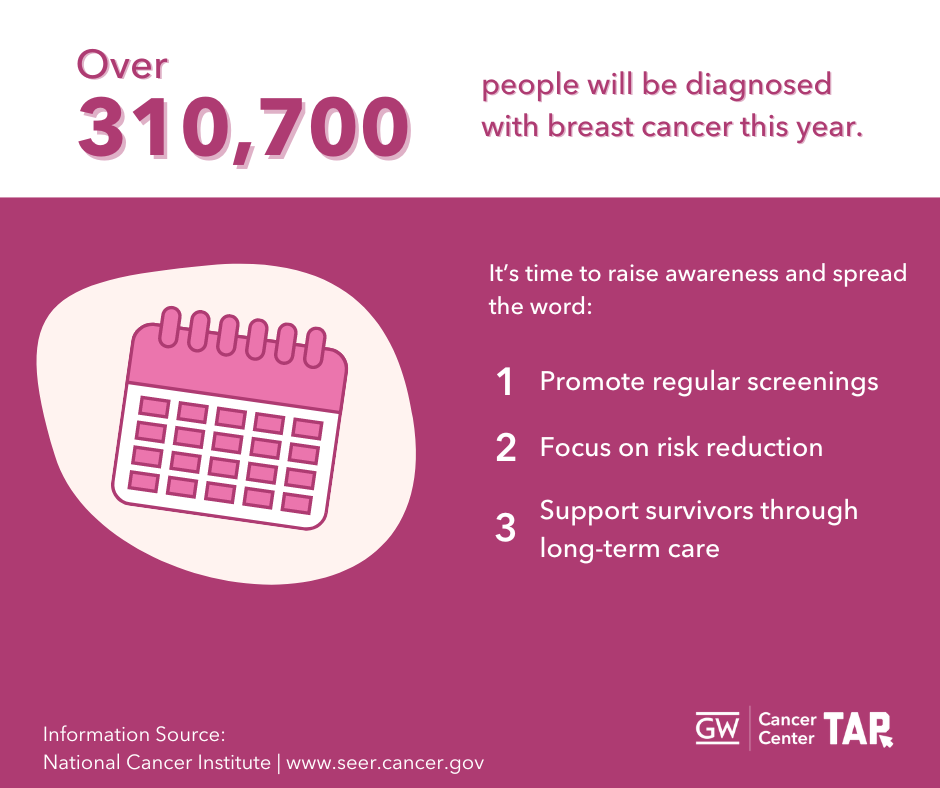 Download Image |
| Talk to your doctor to review your family history and ways to reduce your #breastcancer risk. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Locate a #breastcancer screening provider near you. Find out if you qualify for a free or low-cost mammogram through @cdcgov National Breast and Cervical Cancer Early Detection Program: https://bit.ly/4dUwTYB #TAPintoCancerControl #gwccTAP #TAPforBreastCancer | 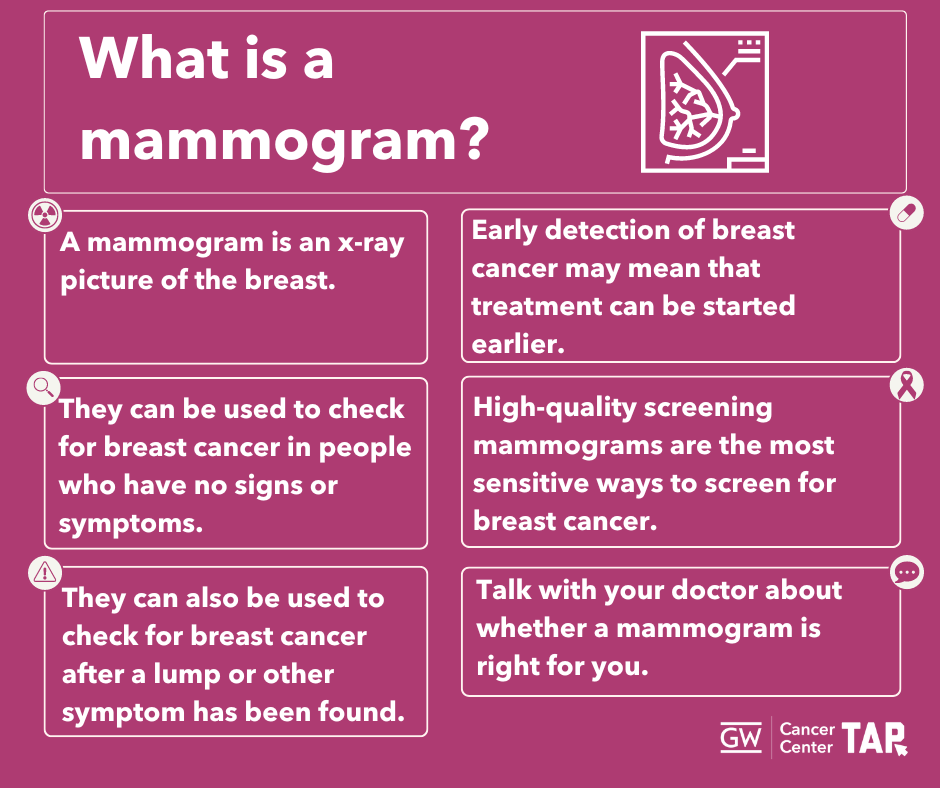 Download Image |
| #Breastcancer clinical trials are critical to improving treatment and creating guidelines for care. Talk to your doctor about whether a trial is right for you @TheNCI’s site: http://bit.ly/329Hhq7 #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| GW offers no-cost training for health professionals on the long-term needs of cancer survivors, including a lesson on #breastcancer. Visit https://bit.ly/3XCKsX0 to learn more. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your breast cancer screening options. Knowing when to start and how often to get screened can make a big difference. #ScreeningSavesLives #BreastHealth #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Did you know that new guidelines from the U.S. Preventive Services Task Force now recommends screening mammography every other year for individuals 40 years old and older? Are you up to date? #ScreeningSavesLives #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer | 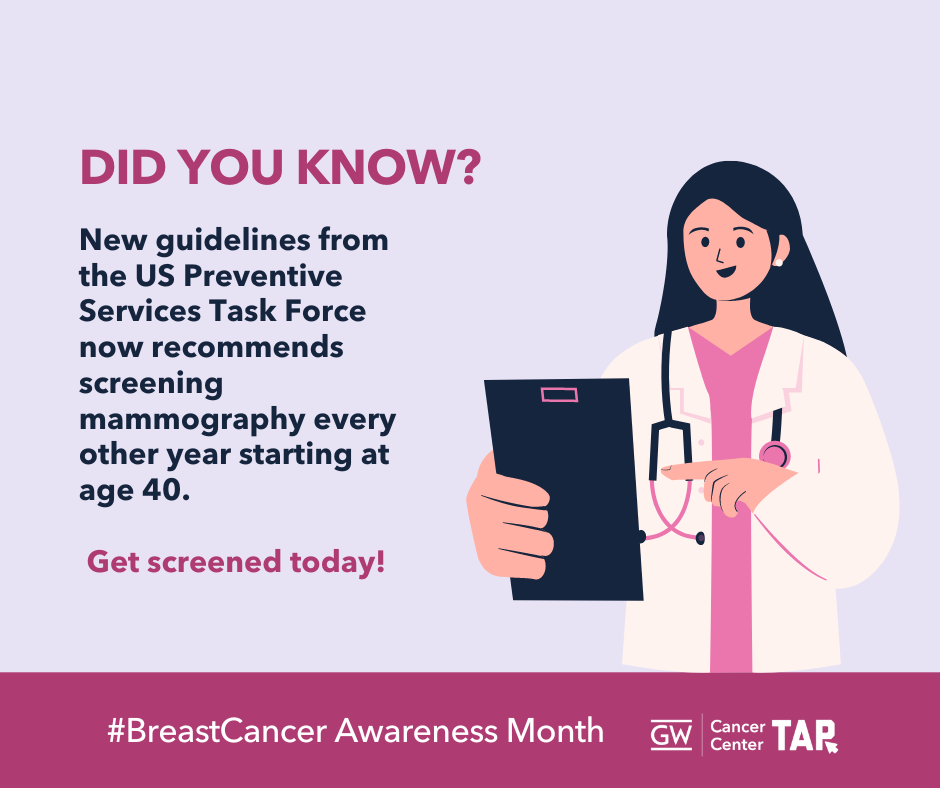 Download Image |
| Under 45? 1 in 10 patients are diagnosed with breast cancer when they are younger than 45. Learn about risk factors, symptoms of breast cancer in young people, and support to get screened: https://bit.ly/35rdmyS #TAPintoCancerControl #gwccTAP #TAPforBreastCancer #BreastCancerAwareness |  Download Image |
| Breast cancer affects everyone. It’s important for LGBTQI+ folks to get screened regularly. Talk to your healthcare provider about your risk and screening options. #LGBTQHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Discuss screening options with your healthcare provider today. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Breast cancer can affect anyone. Talk with your family about your health history and schedule an appointment with your healthcare provider today! #CancerScreening #ScreeningSavesLives #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Talk with your healthcare provider about your family history to create your personalized screening plan. #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Access valuable breast cancer resources in Spanish! Explore @Susan G. Komen’s downloadable resources tailored for the Hispanic community: https://bit.ly/3MHv8lL #HispanicHealth #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Personalized cancer screening is important for everyone. Use this LGBTQI+ guide to create a tailored cancer screening plan from @cedarssinai www.createyourguide.com #LGBTQHealth #CancerScreening #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer as an LGBTQI+ individual? This guide helps LGBTQI+ folks find access and information to breast and chest health. Find support here: https://bit.ly/3AYAnuK #LGBTQHealth #BreastCancerAwareness @Equitas.Health #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Navigating breast cancer can be intimidating for everyone. To get accurate and up-to-date information for your #breastcancer questions, talk to your healthcare provider and get support at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| The @nationalcancerinstitute Cancer Information Service can provide accurate, up-to-date, and reliable information for a range of #breastcancer questions. Learn more at cancer.gov/contact #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Delaying that mammogram because it may cost too much? There is help! Don’t assume you won’t qualify. Check out your state/tribe/territory program: https://bit.ly/3XcDF4Y #EarlyDetection #BreastCancerAwareness #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| Recently diagnosed with #breastcancer? The @NationalCancerInstitute has helpful information on treatment, research, and coping with cancer. Learn more by visiting cancer.gov/types/breast. #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| October is Breast Cancer Awareness Month! Early detection saves lives. Schedule your mammogram today! #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
| It’s Breast Cancer Awareness Month! Talk to your healthcare provider about getting screened today. #BreastCancerAwareness #EarlyDetection #TAPintoCancerControl #gwccTAP #TAPforBreastCancer |  Download Image |
Download All Messages and Graphics
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheet below can be adapted to fit multiple scheduling platforms or services. It is currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Download All Facebook Messages
Download All LinkedIn Messages
Download All Instagram Messages
If you would like to download all images in this social media toolkit, click on each network below for a zip file with each network’s graphics. Please note that these image sizes are slightly smaller than the links above due to file size limitations. If you would like to download full resolution versions, simply click on the “Download Graphic” link below each image in the message tables above.
Download All Facebook Graphics
Download All LinkedIn Graphics
Download All Instagram Graphics
Template Graphics
Need to adjust our designs? Use our Canva Templates for GW TAP’s Breast Cancer Awareness Month Graphics
Footnotes
1. Centers for Disease Control and Prevention. (2024). U.S. cancer statistics female breast cancer stat bite. https://www.cdc.gov/united-states-cancer-statistics/publications/breast-cancer-stat-bite.html ; American Cancer Society. (2022) Breast Cancer Facts & Figures 2022-2024. Atlanta: American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/2022-2024-breast-cancer-fact-figures-acs.pdf
2. U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention. (2024). Cancer statistics data visualization tool, based on 2021 submission data. Retrieved from https://gis.cdc.gov/Cancer/USCS/#/AtAGlance
3. U.S. Cancer Statistics Working Group, 2024.
4. Anderson, J. N., Graff, J. C., Krukowski, R. A., et al. (2021). “Nobody will tell you. You’ve got to ask!”: An examination of patient-provider communication needs and preferences among Black and White women with early-stage breast cancer. Health Communication, 36(11), 1331-1342. https://doi.org/10.1080/10410236.2020.1751383
5. Oprea, N., Ardito, V., & Ciani, O. (2023). Implementing shared decision-making interventions in breast cancer clinical practice: a scoping review. BMC medical informatics and decision making, 23(1), 164. https://doi.org/10.1186/s12911-023-02263-8
6. Gunn, C. M., Maschke, A., Paasche-Orlow, M. K., Kressin, N. R., Schonberg, M. A., & Battaglia, T. A. (2021). Engaging Women with Limited Health Literacy in Mammography Decision-Making: Perspectives of Patients and Primary Care Providers. Journal of general internal medicine, 36(4), 938–945. https://doi.org/10.1007/s11606-020-06213-2 ; Anderson et al., 2021.
7.Orji, A.F., Yamashita, T. Racial disparities in routine health checkup and adherence to cancer screening guidelines among women in the United States of America. Cancer Causes Control 32, 1247–1256 (2021). https://doi.org/10.1007/s10552-021-01475-5
8.Sonnenblick, E. B., Lebron-Zapata, L., Yang, R., Dodelzon, K., Sevilimedu, V., Milch, H., Dialani, V., Dontchos, B. N., Destounis, S., & Grimm, L. (2022). Breast Imaging for Transgender Individuals: Assessment of Current Practice and Needs. Journal of the American College of Radiology, 19(2), 221–231. https://doi.org/10.1016/j.jacr.2021.09.047 ; Anderson, J. N., Paladino, A. J., Robles, A., Krukowski, R. A., & Graetz, I. (2023). “I don’t just say, Hi! I’m gay”: Sexual Orientation Disclosures in Oncology Clinic Settings Among Sexual Minority Women Treated for Breast Cancer in the U.S. South. Seminars in Oncology Nursing, 39(4), 151452. https://doi.org/10.1016/J.SONCN.2023.151452
9.Fung, J., Vang, S., Margolies, L. R., Li, A., Blondeau-Lecomte, E., Li, A., & Jandorf, L. (2021). Developing a culturally and linguistically targeted breast cancer educational program for a multicultural population. Journal of Cancer Education, 36(2), 395-400. https://doi.org/10.1007/s13187-019-01643-x
10.Anderson et al., 2021.
11.Anderson et al., 2021.
12.Black, K. Z., Eng, E., Schaal, J. C., Johnson, L., Nichols, H. B., Ellis, K. R., Rowley, D. L. (2020). The other side of through: Young breast cancer survivors’ spectrum of sexual and reproductive health needs. Qualitative Health Research, 30(13), 2019-2032. https://doi.org/10.1177/1049732320929649
13.Caminiti, C., Diodati, F., Annunziata, M. A., Di Giulio, P., Isa, L., Mosconi, P., Nanni, M. G., Patrini, A., Piredda, M., Santangelo, C., Verusio, C., Cinquini, M., Fittipaldo, V. A., & Passalacqua, R. (2021). Psychosocial Care for Adult Cancer Patients: Guidelines of the Italian Medical Oncology Association. Cancers, 13(19), 4878. https://doi.org/10.3390/cancers13194878 ; Dinapoli, L., Colloca, G., Di Capua, B., & Valentini, V. (2021). Psychological Aspects to Consider in Breast Cancer Diagnosis and Treatment. Current oncology reports, 23(3), 38. https://doi.org/10.1007/s11912-021-01049-3
14.Ben-Ari, E. (2022). Meeting cancer survivors’ psychosocial health needs: A conversation with Dr. Patricia Ganz. National Cancer Institute. https://www.cancer.gov/news-events/cancer-currents-blog/2022/psychosocial-cancer-survivors-patricia-ganz
15.Rositch, A. F., Unger-Saldaña, K., DeBoer, R. J., Ng’ang’a, A., & Weiner, B. J. (2020). The role of dissemination and implementation science in global breast cancer control programs: Frameworks, methods, and examples. Cancer, 126(10), 2394-2404. https://doi.org/10.1002/cncr.32877
16.National Cancer Institute. (2024). Cancer disparities. Retrieved from https://www.cancer.gov/about-cancer/understanding/disparities ; Alcaraz, K. I., Wiedt, T. L., Daniels, E. C., Yabroff, K. R., Guerra, C. E., & Wender, R. C. (2020). Understanding and addressing social determinants to advance cancer health equity in the United States: A blueprint for practice, research, and policy. CA: A Cancer Journal for Clinicians, 70(1), 31-46. https://doi.org/10.3322/caac.21586
17.National Cancer Institute, 2024.
18.National Cancer Institute, 2024 ; Stringer-Reasor, E. M., Elkhanany, A., Khoury, K., Simon, M. A., & Newman, L. A. (2021). Disparities in Breast Cancer Associated With African American Identity. Journal of Oncology Practice, 41, e29-e46. https://doi.org/10.1200/EDBK_319929
19.Wilson, J., & Sule, A. A. (2020). Disparity in Early Detection of Breast Cancer. StatPearls. http://europepmc.org/books/NBK564311
20.Wilson and Sule, 2020.
21.Yedjou, C. G., Sims, J. N., Miele, L., Noubissi, F., Lowe, L., Fonsca, D. D., Alo, R. A., Payton, M., and Tchounwou, P. B. (2019). Health and racial disparity in breast cancer. Breast Cancer Metastasis and Drug Resistance, 31-40.
22.Mouslim, M.C., Johnson, R.M. & Dean, L.T. (2020). Healthcare system distrust and the breast cancer continuum of care. Breast Cancer Res Treat 180, 33–44. https://doi.org/10.1007/s10549-020-05538-0
23.Wilson and Sule, 2020.
24.American Cancer Society. (2021). Cancer Facts & Figures for Hispanic/Latino People 2021-2023. Atlanta: American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/hispanic-latino-2021-2023-cancer-facts-and-figures.pdf ; Yedjou et al., 2019.
25.ACS, 2021.
26.Cohen, R. A., & Cha, A. E. (2023). Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2022. National Center for Health Statistics. https://dx.doi.org/10.15620/cdc:127055
27.Ko NY, Hong S, Winn RA, Calip GS. (2020). Association of Insurance Status and Racial Disparities With the Detection of Early-Stage Breast Cancer. JAMA Oncol. 6(3):385–392. doi:10.1001/jamaoncol.2019.5672
28.Talham, C. J., Montiel Ishino, F. A., O’Brien, K. M., Sandler, D. P., & Williams, F. (2022). Breast cancer screening among Hispanic and non-Hispanic White women by birthplace in the Sister Study. Cancer medicine, 11(8), 1913–1922. https://doi.org/10.1002/cam4.4563
29.Talham et al., 2022.
30.Talham et al., 2022.
31.Bonilla, J., Escalera, C., Santoyo-Olsson, J., Samayoa, C., Ortiz, C., Stewart, A. L., & Nápoles, A. M. (2021). The importance of patient engagement to quality of breast cancer care and health-related quality of life: a cross-sectional study among Latina breast cancer survivors in rural and urban communities. BMC women’s health, 21(1), 59. https://doi.org/10.1186/s12905-021-01200-z
32.Reddy, S., Saxon, M., Patel, N., Speer, M., Ziegler, T., Patel, N., Ziegler, M., Esquivel, S., Mata, A. D., Devineni, A., Paode, P., Thawani, N., & Mutyala, S. (2020). Discordance in Perceptions of Barriers to Breast Cancer Treatment Between Hispanic Women and Their Providers. Journal of patient-centered research and reviews, 7(4), 337–342.
33.Centers for Disease Control and Prevention. (2019). Breast cancer in young women. https://www.cdc.gov/bring-your-brave/breast-cancer-in-young-women/index.html
34.CDC, 2019.
35.Vollmer Dahlke, D., Yoshikawa, A., McAdam, M., Malatok, S., & Gonzales, E. D. (2022). An Analysis of Health Care Team Communication Needs Among Younger vs Older Breast Cancer Survivors: Web-Based Survey. JMIR cancer, 8(1), e31118. https://doi.org/10.2196/31118
36.Monticciolo, D. L., Newell, M. S., Moy, L., Lee, C. S., & Destounis, S. V. (2023). Breast Cancer Screening for Women at Higher-Than-Average Risk: Updated Recommendations From the ACR. Journal of the American College of Radiology : JACR, 20(9), 902–914. https://doi.org/10.1016/j.jacr.2023.04.002
37.American Cancer Society Cancer Action Network. (2023). Survivor Views: LGBTQ+ Cancer Patients & Survivors. Atlanta: American Cancer Society, Inc. https://www.fightcancer.org/sites/default/files/national_documents/lgbtq_patient_discrimination_0.pdf
38.Kiran, T., Davie, S., Singh, D., Hranilovic, S., Pinto, A. D., Abramovich, A., & Lofters, A. (2019). Cancer screening rates among transgender adults: Cross-sectional analysis of primary care data. Canadian Family Physician, 65(1), 30-37. PMID: 30674526; PMCID: PMC6347308.
39.ACS Cancer Action Network, 2023.
40.Anderson, J. N., Paladino, A. J., Robles, A., Krukowski, R. A., & Graetz, I. (2023). “I don’t just say, Hi! I’m gay”: Sexual Orientation Disclosures in Oncology Clinic Settings Among Sexual Minority Women Treated for Breast Cancer in the U.S. South. Seminars in Oncology Nursing, 39(4), 151452. https://doi.org/10.1016/J.SONCN.2023.151452
41.American Cancer Society. (2024). Cancer Facts & Figures for Asian American, Native Hawaiian & Other Pacific Islander People 2024-2026. Atlanta: American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/aanhpi-cancer-facts-and-figures/aanhpi-cff.pdf
42.Yom, S., Lor, M. Advancing Health Disparities Research: The Need to Include Asian American Subgroup Populations. J. Racial and Ethnic Health Disparities 9, 2248–2282 (2022). https://doi.org/10.1007/s40615-021-01164-8
43.Jun, J. (2020). Cancer/health communication and breast/cervical cancer screening among Asian Americans and five Asian ethnic groups. Ethnicity & Health, 25(7), 960-981. https://doi.org/10.1080/13557858.2018.1478952
44.ACS, 2024; Taparra et al. (2022). Disaggregation of Asian American and Pacific Islander Women With Stage 0-II Breast Cancer Unmasks Disparities in Survival and Surgery-to-Radiation Intervals: A National Cancer Database Analysis From 2004 to 2017. JCO Oncology Practice, 18, 1255-1264. https://doi.org/10.1200/OP.22.00001
45.ACS, 2024.
46.Taparra et al., 2022.
47.Moss, J. L., Pinto, C. N., Srinivasan, S., Cronin, K. A., & Croyle, R. T. (2020). Persistent Poverty and Cancer Mortality Rates: An Analysis of County-Level Poverty Designations. Cancer Epidemiology Biomarkers & Prevention, 29(10), 1949-1954. https://doi.org/10.1158/1055-9965.EPI-20-0007
48.Kenzik, K. M., Rocque, G. B., Landier, W., & Bhatia, S. (2020). Urban versus Rural Residence and Outcomes in Older Patients with Breast Cancer. Cancer Epidemiology Biomarkers & Prevention, 29(7), 1313-1320. https://doi.org/10.1158/1055-9965.EPI-19-1414
49.Papageorge, M. V., Woods, A. P., de Geus, S. W. L., Ng, S. C., McAneny, D., Tseng, J. F., Kenzik, K. M., & Sachs, T. E. (2023). The persistence of poverty and its impact on cancer diagnosis, treatment, and survival. Annals of Surgery, 277(6), 995-1001. https://doi.org/10.1097/SLA.0000000000005455
50.Yedjou et al., 2019.
51.Berrian, J. L., Liu, Y., Lian, M., Schmaltz, C. L., & Colditz, G. A. (2021). Relationship between insurance status and outcomes for patients with breast cancer in Missouri. Cancer, 127(6), 931-937. https://doi.org/10.1002/cncr.33330
References
Al Shamsi, H., Almutairi, A. G., Al Mashrafi, S., & Al Kalbani, T. (2020). Implications of language barriers for healthcare: A systematic review. Oman Medical Journal, 35(2), e122. https://doi.org/10.5001/omj.2020.40
Alcaraz, K. I., Wiedt, T. L., Daniels, E. C., Yabroff, K. R., Guerra, C. E., & Wender, R. C. (2020). Understanding and addressing social determinants to advance cancer health equity in the United States: A blueprint for practice, research, and policy. CA: A Cancer Journal for Clinicians, 70(1), 31-46. https://doi.org/10.3322/caac.21586
American Cancer Society. (2021). Cancer Facts & Figures for Hispanic/Latino People 2021-2023. Atlanta: American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/hispanic-latino-2021-2023-cancer-facts-and-figures.pdf
American Cancer Society. (2022) Breast Cancer Facts & Figures 2022-2024. Atlanta: American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/2022-2024-breast-cancer-fact-figures-acs.pdf
American Cancer Society Cancer Action Network. (2023). Survivor Views: LGBTQ+ Cancer Patients & Survivors. Atlanta: American Cancer Society, Inc. https://www.fightcancer.org/sites/default/files/national_documents/lgbtq_patient_discrimination_0.pdf
American Cancer Society. (2024). Cancer Facts & Figures for Asian American, Native Hawaiian & Other Pacific Islander People 2024-2026. Atlanta: American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/aanhpi-cancer-facts-and-figures/aanhpi-cff.pdf
American College of Radiology. (2021). ACR Appropriateness Criteria: Transgender Breast Cancer Screening. https://acsearch.acr.org/docs/3155692/Narrative/
Anderson, J. N., Graff, J. C., Krukowski, R. A., et al. (2021). “Nobody will tell you. You’ve got to ask!”: An examination of patient-provider communication needs and preferences among Black and White women with early-stage breast cancer. Health Communication, 36(11), 1331-1342. https://doi.org/10.1080/10410236.2020.1751383
Anderson, J. N., Paladino, A. J., Robles, A., Krukowski, R. A., & Graetz, I. (2023). “I don’t just say, Hi! I’m gay”: Sexual Orientation Disclosures in Oncology Clinic Settings Among Sexual Minority Women Treated for Breast Cancer in the U.S. South. Seminars in Oncology Nursing, 39(4), 151452. https://doi.org/10.1016/J.SONCN.2023.151452
Ben-Ari, E. (2022). Meeting cancer survivors’ psychosocial health needs: A conversation with Dr. Patricia Ganz. National Cancer Institute. https://www.cancer.gov/news-events/cancer-currents-blog/2022/psychosocial-cancer-survivors-patricia-ganz
Berrian, J. L., Liu, Y., Lian, M., Schmaltz, C. L., & Colditz, G. A. (2021). Relationship between insurance status and outcomes for patients with breast cancer in Missouri. Cancer, 127(6), 931-937. https://doi.org/10.1002/cncr.33330
Black, K. Z., Eng, E., Schaal, J. C., Johnson, L., Nichols, H. B., Ellis, K. R., Rowley, D. L. (2020). The other side of through: Young breast cancer survivors’ spectrum of sexual and reproductive health needs. Qualitative Health Research, 30(13), 2019-2032. https://doi.org/10.1177/1049732320929649
Bonilla, J., Escalera, C., Santoyo-Olsson, J., Samayoa, C., Ortiz, C., Stewart, A. L., & Nápoles, A. M. (2021). The importance of patient engagement to quality of breast cancer care and health-related quality of life: a cross-sectional study among Latina breast cancer survivors in rural and urban communities. BMC women’s health, 21(1), 59. https://doi.org/10.1186/s12905-021-01200-z
Caminiti, C., Diodati, F., Annunziata, M. A., Di Giulio, P., Isa, L., Mosconi, P., Nanni, M. G., Patrini, A., Piredda, M., Santangelo, C., Verusio, C., Cinquini, M., Fittipaldo, V. A., & Passalacqua, R. (2021). Psychosocial Care for Adult Cancer Patients: Guidelines of the Italian Medical Oncology Association. Cancers, 13(19), 4878. https://doi.org/10.3390/cancers13194878
Champion, V. L., Paskett, E. D., Stump, T. E., et al. (2023). Comparative effectiveness of 2 interventions to increase breast, cervical, and colorectal cancer screening among women in the rural US: A randomized clinical trial. JAMA Network Open, 6(4), e2311004. https://doi.org/10.1001/jamanetworkopen.2023.11004
Centers for Disease Control and Prevention. (2024). Basic information about breast cancer. https://www.cdc.gov/breast-cancer/about/index.html
Centers for Disease Control and Prevention. (2019). Breast cancer in young women. https://www.cdc.gov/bring-your-brave/breast-cancer-in-young-women/index.html
Centers for Disease Control and Prevention. (2024). Screening for breast cancer. https://www.cdc.gov/breast-cancer/screening/index.html
Centers for Disease Control and Prevention. (2024). U.S. cancer statistics female breast cancer stat bite. https://www.cdc.gov/united-states-cancer-statistics/publications/breast-cancer-stat-bite.html
Cohen, R. A., & Cha, A. E. (2023). Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2022. National Center for Health Statistics. https://dx.doi.org/10.15620/cdc:127055
Dinapoli, L., Colloca, G., Di Capua, B., & Valentini, V. (2021). Psychological Aspects to Consider in Breast Cancer Diagnosis and Treatment. Current oncology reports, 23(3), 38. https://doi.org/10.1007/s11912-021-01049-3
Fung, J., Vang, S., Margolies, L. R., Li, A., Blondeau-Lecomte, E., Li, A., & Jandorf, L. (2021). Developing a culturally and linguistically targeted breast cancer educational program for a multicultural population. Journal of Cancer Education, 36(2), 395-400. https://doi.org/10.1007/s13187-019-01643-x
Gunn, C. M., Maschke, A., Paasche-Orlow, M. K., Kressin, N. R., Schonberg, M. A., & Battaglia, T. A. (2021). Engaging Women with Limited Health Literacy in Mammography Decision-Making: Perspectives of Patients and Primary Care Providers. Journal of general internal medicine, 36(4), 938–945. https://doi.org/10.1007/s11606-020-06213-2
Jun, J. (2020). Cancer/health communication and breast/cervical cancer screening among Asian Americans and five Asian ethnic groups. Ethnicity & Health, 25(7), 960-981. https://doi.org/10.1080/13557858.2018.1478952
Kenzik, K. M., Rocque, G. B., Landier, W., & Bhatia, S. (2020). Urban versus Rural Residence and Outcomes in Older Patients with Breast Cancer. Cancer Epidemiology Biomarkers & Prevention, 29(7), 1313-1320. https://doi.org/10.1158/1055-9965.EPI-19-1414
Kiran, T., Davie, S., Singh, D., Hranilovic, S., Pinto, A. D., Abramovich, A., & Lofters, A. (2019). Cancer screening rates among transgender adults: Cross-sectional analysis of primary care data. Canadian Family Physician, 65(1), 30-37. PMID: 30674526; PMCID: PMC6347308.
Ko NY, Hong S, Winn RA, Calip GS. (2020). Association of Insurance Status and Racial Disparities With the Detection of Early-Stage Breast Cancer. JAMA Oncol. 6(3):385–392. doi:10.1001/jamaoncol.2019.5672
Monticciolo, D. L., Newell, M. S., Moy, L., Lee, C. S., & Destounis, S. V. (2023). Breast Cancer Screening for Women at Higher-Than-Average Risk: Updated Recommendations From the ACR. Journal of the American College of Radiology : JACR, 20(9), 902–914. https://doi.org/10.1016/j.jacr.2023.04.002
Moss, J. L., Pinto, C. N., Srinivasan, S., Cronin, K. A., & Croyle, R. T. (2020). Persistent Poverty and Cancer Mortality Rates: An Analysis of County-Level Poverty Designations. Cancer Epidemiology Biomarkers & Prevention, 29(10), 1949-1954. https://doi.org/10.1158/1055-9965.EPI-20-0007
Mouslim, M.C., Johnson, R.M. & Dean, L.T. (2020). Healthcare system distrust and the breast cancer continuum of care. Breast Cancer Res Treat 180, 33–44. https://doi.org/10.1007/s10549-020-05538-0
National Cancer Institute. (2024). Cancer disparities. Retrieved from https://www.cancer.gov/about-cancer/understanding/disparities
Oprea, N., Ardito, V., & Ciani, O. (2023). Implementing shared decision-making interventions in breast cancer clinical practice: a scoping review. BMC medical informatics and decision making, 23(1), 164. https://doi.org/10.1186/s12911-023-02263-8
Orji, A.F., Yamashita, T. (2021). Racial disparities in routine health checkup and adherence to cancer screening guidelines among women in the United States of America. Cancer Causes Control 32, 1247–1256. https://doi.org/10.1007/s10552-021-01475-5
Papageorge, M. V., Woods, A. P., de Geus, S. W. L., Ng, S. C., McAneny, D., Tseng, J. F., Kenzik, K. M., & Sachs, T. E. (2023). The persistence of poverty and its impact on cancer diagnosis, treatment, and survival. Annals of Surgery, 277(6), 995-1001. https://doi.org/10.1097/SLA.0000000000005455
Reddy, S., Saxon, M., Patel, N., Speer, M., Ziegler, T., Patel, N., Ziegler, M., Esquivel, S., Mata, A. D., Devineni, A., Paode, P., Thawani, N., & Mutyala, S. (2020). Discordance in Perceptions of Barriers to Breast Cancer Treatment Between Hispanic Women and Their Providers. Journal of patient-centered research and reviews, 7(4), 337–342.Rositch, A. F., Unger-Saldaña, K., DeBoer, R. J., Ng’ang’a, A., & Weiner, B. J. (2020). The role of dissemination and implementation science in global breast cancer control programs: Frameworks, methods, and examples. Cancer, 126(10), 2394-2404. https://doi.org/10.1002/cncr.32877
Sonnenblick, E. B., Lebron-Zapata, L., Yang, R., Dodelzon, K., Sevilimedu, V., Milch, H., Dialani, V., Dontchos, B. N., Destounis, S., & Grimm, L. (2022). Breast Imaging for Transgender Individuals: Assessment of Current Practice and Needs. Journal of the American College of Radiology, 19(2), 221–231. https://doi.org/10.1016/j.jacr.2021.09.047
Stringer-Reasor, E. M., Elkhanany, A., Khoury, K., Simon, M. A., & Newman, L. A. (2021). Disparities in Breast Cancer Associated With African American Identity. Journal of Oncology Practice, 41, e29-e46. https://doi.org/10.1200/EDBK_319929
Suarez, A., Bisschops, J., & Lampen-Sachar, K. (2024). Breast Cancer Screening Recommendations for Transgender Patients: A Review. Mayo Clinic Proceedings, 99(4), 630–639. https://doi.org/10.1016/j.mayocp.2023.12.006
Talham, C. J., Montiel Ishino, F. A., O’Brien, K. M., Sandler, D. P., & Williams, F. (2022). Breast cancer screening among Hispanic and non-Hispanic White women by birthplace in the Sister Study. Cancer medicine, 11(8), 1913–1922. https://doi.org/10.1002/cam4.4563
Taparra et al. (2022). Disaggregation of Asian American and Pacific Islander Women With Stage 0-II Breast Cancer Unmasks Disparities in Survival and Surgery-to-Radiation Intervals: A National Cancer Database Analysis From 2004 to 2017. JCO Oncology Practice, 18, 1255-1264. https://doi.org/10.1200/OP.22.00001
U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention. (2024). Cancer statistics data visualization tool, based on 2021 submission data. Retrieved from https://gis.cdc.gov/Cancer/USCS/#/AtAGlance
Vollmer Dahlke, D., Yoshikawa, A., McAdam, M., Malatok, S., & Gonzales, E. D. (2022). An Analysis of Health Care Team Communication Needs Among Younger vs Older Breast Cancer Survivors: Web-Based Survey. JMIR cancer, 8(1), e31118. https://doi.org/10.2196/31118
Warren, G. W., Alberg, A. J., Cummings, K. M., & Dresler, C. (2020). Smoking Cessation After a Cancer Diagnosis Is Associated With Improved Survival. Journal of Thoracic Oncology, 15(5), 705–708. https://doi.org/10.1016/j.jtho.2020.02.002
Wilson, J., & Sule, A. A. (2020). Disparity in Early Detection of Breast Cancer. StatPearls. http://europepmc.org/books/NBK564311
Yedjou, C. G., Sims, J. N., Miele, L., Noubissi, F., Lowe, L., Fonsca, D. D., Alo, R. A., Payton, M., and Tchounwou, P. B. (2019). Health and racial disparity in breast cancer. Breast Cancer Metastasis and Drug Resistance, 31-40.
Yom, S., Lor, M. (2022). Advancing Health Disparities Research: The Need to Include Asian American Subgroup Populations. J. Racial and Ethnic Health Disparities 9, 2248–2282. https://doi.org/10.1007/s40615-021-01164-8

